July 16, 2018 — A four-protein biomarker blood test improves lung cancer risk assessment over existing guidelines that rely solely upon smoking history. The blood test captures risk for people who have ever smoked, not only for heavy smokers, an international research team reports in JAMA Oncology.
“This simple blood test demonstrates the potential of biomarker-based risk assessment to improve eligibility criteria for lung cancer screening with low-dose computed tomography,” said study co-senior author Sam Hanash, M.D., Ph.D., professor of clinical cancer prevention at The University of Texas MD Anderson Cancer Center.
The biomarker panel achieved superior sensitivity – identification of smokers who later developed lung cancer – without increasing false-positives compared to guidelines for screening approved by the U.S. Preventive Service Task Force (USPSTF) for heavy smokers based on age and smoking history.
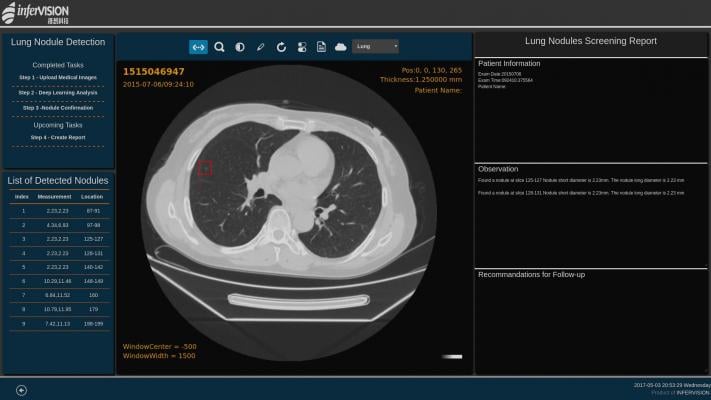
USPSTF guidelines call for computed tomography (CT) screening only of adults between ages 55 and 80 with a 30 pack-year smoking history who either smoke or have quit within the past 15 years.
“The biomarker panel more accurately identifies at-risk smokers who should proceed to screening, even if they’re not at the highest risk based on smoking history alone,” Hanash said. “A positive blood test means an ever-smoker is as much, if not more so, at risk of having lung cancer as a heavy smoker with a low biomarker score.”
The paper reports a validation study of the biomarker model in 63 ever-smoking patients who developed lung cancer within a year of initial blood sample collection compared to 90 matched controls in two large European population-based cohorts.
Researchers compared a model based on smoking history to an integrated model that included the biomarker score based on the four markers plus smoking history.
At the same level of false-positive rate (specificity) set by the USPSTF guidelines, the integrated test with biomarkers identified 63 percent of future lung cancer cases (40 of 63), compared to 42 percent (20 of 62) based on smoking history alone.
The improved detection rate, Hanash said, reflects the biomarker panel’s ability to identify at-risk people among the larger population of ever-smokers. In the validation study, smoking history did not improve prediction of future lung cancer cases beyond that provided by the biomarkers alone.
Hanash said the key to selecting the biomarkers was the availability of blood samples taken from people before they had developed the disease. This contrasts to most previous studies comparing biomarkers in early-stage lung cancer patients to healthy controls. Such studies do not reflect how biomarkers can help to predict future cancers.
To develop the biomarker blood test, Hanash’s group led the analysis of blood samples taken from 108 ever-smokers who went on to be diagnosed with lung cancer within a year of sampling, compared to 216 smoking-matched controls. All were participants in the Carotene and Retinol Efficacy Trial (CARET), a lung cancer prevention trial conducted in North America in the 1990s.
“We compared smokers with lung cancer to smokers who didn’t have lung cancer, and we showed there are biomarker differences between those groups, so it wasn’t only smoking status giving us differences,” Hanash said. “Then we compared cancer cases to the general population and found similar differences.”
The resulting panel includes four proteins found in the blood:
- The precursor form of surfactant protein B (Pro-SFTPB);
- Cancer antigen 125 (CA125);
- Cytokeratin-19 fragment (CYFRA 21-1); and
- Carcinoembryonic antigen (CEA).
The validation study was conducted among patients from the European Prospective Investigation into Cancer and Nutrition and the Northern Sweden Health and Disease Study.
The researchers note that their findings need to be validated in larger studies to further validate and fine-tune the biomarker-based prediction model. Hanash said that will depend upon guidance from the U.S. Food and Drug Administration (FDA), and consultations with the FDA have begun.
Lung cancer causes an estimated 20-25 percent of all deaths from cancer — 1.69 million annually worldwide and 155,000 in the United States. Early detection improves prospects of survival, but most countries do not screen for the disease and it’s estimated that fewer than half of all U.S. cases are among people who are eligible under USPSTF guidelines.
For more information: www.jamanetwork.com/journals/jamaoncology
Reference


 February 11, 2026
February 11, 2026 









