Photo: Children’s Hospital Los Angeles
Oct. 28, 2025 — Bronchopulmonary dysplasia (BPD) is the most common — and most serious — complication of extreme prematurity. Yet clinicians still lack a reliable way to measure the severity of the disease or predict which infants will need long-term respiratory support.
Now, researchers at Children’s Hospital Los Angeles (CHLA) are investigating low-field MRI to safely capture both lung structure and function in these babies — offering a new window into how their fragile lungs develop.
“Low-field MRI is a revolution in the lung imaging field,” says Narayan Iyer, MD, a neonatologist in the Fetal and Neonatal Institute and principal investigator of the study. “This is the one imaging tool that can show you not only how the lung looks, but also how it works. That’s what makes this so exciting.”
Building on BPD Expertise
CHLA is an ideal place to explore new tools for understanding and treating BPD. Its Infant Chronic Lung Disease Program treats nearly 70 patients a year and is one of the leading programs in the country for babies with severe BPD.
Earlier this year, CHLA also became the first pediatric hospital in the nation to acquire a low-field MRI machine, the Siemens FreeMax 0.55 Tesla MRI. Although the machine is housed in the hospital’s state-of-the-art Cardiac Imaging Suite, one of its most powerful potential applications is lung imaging.
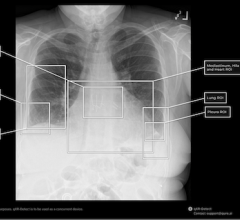
The need for this new imaging is great. While CT scans can provide detailed pictures of lung structure, they can’t capture lung function. They also expose patients to radiation, making them unsuitable for routine use in infants.
That leaves clinicians with little way to measure BPD’s severity. “It’s like listening to the lungs with a stethoscope you’re not wearing,” says Roberta Kato, MD, a pediatric pulmonologist with Pulmonology and Sleep Medicine and an investigator on the study. “We’re just not getting any information that helps stratify the patient’s disease.”
Linking Scans to Outcomes
The CHLA team has already enrolled 10 babies in the feasibility portion of its study. Eligible patients must be born at 32 weeks’ gestation or earlier and have a significant need for oxygen or a breathing machine.
Once the infants reach what would have been their 40-week due date, their lungs are imaged with the low-field MRI machine. No anesthesia is needed; babies typically sleep through the 10-to-15-minute scan.
In addition to imaging the lungs’ structure, the scan uses special techniques to assess lung function. One approach, called phase-resolved functional lung scan (PREFUL), spatially quantifies airflow and blood flow through the lungs. Two MRI scientists at CHLA, Xin Miao, PhD, and Eamon Doyle, PhD, are also spearheading the technical development of novel MRI techniques.
Researchers then link data from the scans to each baby’s clinical outcome, including length of hospital stay and whether the baby ends up needing a tracheostomy or long-term ventilatory support. The team is also identifying which MRI sequences are most informative.
If results are successful, the earliest clinical applications for BPD could be seen within three to five years, Dr. Iyer says.
“Right now we treat all babies with BPD the same way, even though their lung disease is different,” he notes. “The goal is to use MRI to predict which babies end up with more severe disease. That would allow us to intervene much earlier in high-risk patients and finally individualize care.”
Watching Lungs Recover
Once the feasibility portion is complete, researchers hope to expand the study to all CHLA patients with BPD. Future phases plan to incorporate serial scans to watch lungs develop and recover in real time.
Because lungs continue developing well into adolescence, the team sees a critical opportunity to better understand—and eventually support—these recovery processes. Low-field MRI could also transform clinical research for BPD.
“Having a quantifiable way to measure lung function in these babies would provide clinical trial endpoints that would allow us to assess if a novel or existing therapy is effective,” Dr. Kato explains.
And while this study is focused on BPD, low-field MRI could also one day aid children with cystic fibrosis, asthma, or cancer, or even adults with chronic obstructive pulmonary disease (COPD).
“We’re still early in our research,” notes Dr. Iyer. “Our ultimate goal is to use this technology to transform care for babies with BPD, and eventually, many other young patients with lung disease.”


 March 06, 2026
March 06, 2026