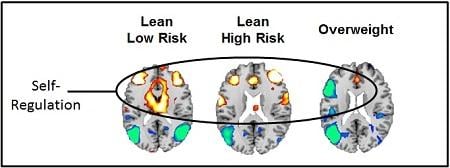
Increased brain activity when viewing food cues shown in yellow, orange, and red. Decreased activity is shown in blue. Activations are present in circuits that support self-regulation and attention (frontal cortex, anterior cingulate and basal ganglia). Image courtesy of Bradley Peterson, M.D., Children’s Hospital Los Angeles.
August 28, 2017 — A team of researchers recently used functional magnetic resonance imaging (fMRI) to investigate neural responses to food cues in overweight compared with lean adolescents. The team, including senior investigator Bradley Peterson, M.D., director of the Institute for the Developing Mind at Children’s Hospital Los Angeles, observed that food stimuli activated regions of the brain associated with reward and emotion in all groups. However, adolescents at an increasing risk for obesity had progressively less neural activity in circuits of the brain that support self-regulation and attention.
“This study establishes that risk for obesity isn’t driven exclusively by the absence or presence of urges to eat high-calorie foods, but also, and perhaps most importantly, by the ability to control those urges,” said Peterson, who is also a professor at the Keck School of Medicine at the University of Southern California.
The public health implications of childhood obesity are staggering. More than half of all adolescents in the U.S. are either overweight or obese. Children of overweight parents (2/3 of adults in the U.S.) already are or are likely to become overweight. Since excess weight has been linked to a myriad of health issues shown to limit human potential and add to the skyrocketing cost of healthcare, researchers are actively seeking novel approaches to understand better the causes of obesity and alter its trajectory. This study, recently reported in the journal NeuroImage, may offer such an approach.
“We wanted to use brain imaging to investigate a key question in obesity science: Why do some people become obese, while others don’t?” said Susan Carnell, Ph.D., assistant professor of child and adolescent psychiatry, Johns Hopkins University School of Medicine and first author on the study.
Of the 36 adolescents (ages 14 to 19 years) enrolled in the study, 10 were overweight/obese, 16 were lean but considered at high risk for obesity because they had overweight/obese mothers, and 10 were lean/low risk since they had lean mothers. The adolescents underwent brain scanning using fMRI, while they viewed words that described high-fat foods, low-fat foods and non-food items. Then they rated their appetite in response to each word stimulus. Following the activity, all participants were offered a buffet that included low- and high-calorie foods — to relate participants test responses to real-world behavior.
The investigators observed that after viewing food-related words, brain circuits that support reward and emotion were stimulated in all participants. In adolescents who were obese or who were lean but at high familial risk for obesity, they observed less activation in attention and self-regulation circuits.
Brain circuits that support attention and self-regulation showed the greatest activation in lean/low-risk adolescents, less activity in lean/high-risk participants and least activation in the overweight/obese group. Also, real world relevance mirrored fMRI findings — food intake at the buffet was greatest in the overweight/obese participants, followed by the lean/high-risk adolescents and lowest in the lean/low-risk group.
“These findings suggest that interventions designed to stimulate the self-regulatory system in adolescents may provide a new approach for treating and preventing obesity,” said Peterson.
Additional contributors to the study include Leora Benson, Johns Hopkins University School of Medicine; Ky-Yu (Virginia) Chang and Allan Geliebter, Icahn School of Medicine; and Zhishun Wang and Yuankai Huo, Columbia University Medical Center. The study was supported in part by NIDDK (K99R00DK088360, R01DK074046 and DK080153).
For more information: www.journals.elsevier.com/neuroimage


 February 13, 2026
February 13, 2026 









