
Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.
BLOG: Why Power Injectors Are Needed for High-Quality Imaging
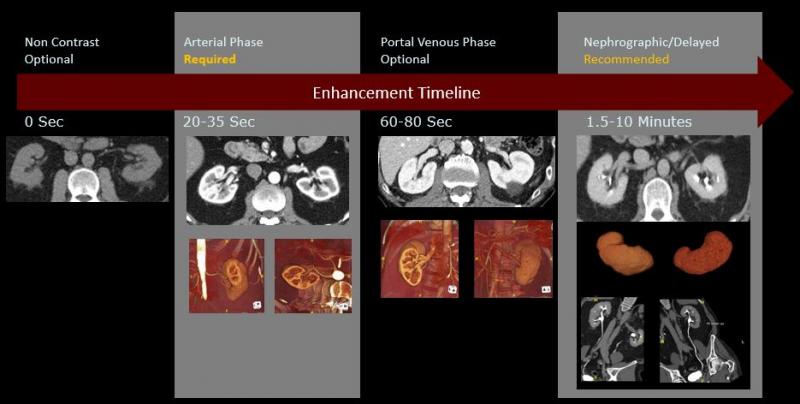
Image courtesy of Lior Molvin
Contrast agents improve every kind of medical image from computed tomography (CT) to magnetic resonance imaging (MR), radiography and fluoroscopy to ultrasound. Whether these exams are diagnostic depends directly on the proper injection of these media.
Lior Molvin, a CT technologist and protocol manager for the diagnostic CT group at Stanford Health Care, noted that nondiagnostic results waste the time of the patient, hospital staff and radiologist; and can throw a monkey wrench into scheduling, if a repeat exam is needed. They waste money and may needlessly expose the patient to radiation. Worst of all, they can critically delay treatment.
Power injectors can directly impact image quality and patient safety, said the CT protocol manager, who began as a technologist in 2006 at the Stanford University Medical Center. Over that time, Molvin has gained extensive experience with hospital and outpatient diagnostic equipment. Among his specialties are CT protocol optimization, technologist education and radiation safety.
The Power of the Injector
Only through the use of power injectors can contrast agents be administered at exactly the times and the flow rates needed to consistently achieve high-quality images, he said. When combined with pressure monitoring systems and hardware to prevent extravasation — defined as the accidental leakage of IV material into the surrounding tissue — these injectors can simultaneously mitigate risk.
But to be effective, technologists must consider the limitations of these machines. The jet of contrast coming from the injector can dislodge the needle from inside the vein, causing extravasation. While extravasation occurs very infrequently and complications usually are minimal, complications can be severe in extreme cases.
The information to help prevent this from happening can be obtained from a manual test conducted before the CT procedure to determine whether the IV injection and the blood vessel are compatible, Molvin said. Some subtle findings might come from this test. And technologists have to be ready to act on them.
“Let’s say the protocol requires an injection of 6 mLs per second but the manual test reveals the patient would likely experience discomfort at that rate,” he said. “You could reduce the injection rate to 4mLs a second and adjust technical factors on your CT scanner to maintain image quality,” for example, the scan time and kVP.
Technologists must also consider such other issues as the concentration of the medium. High concentrations tend to produce high-quality images. “Isovue 370 always produces images that look better than 350, which look better than 320, which look better than 300,” Molvin said. “But there are times when a lower concentration is merited.”
Viscosity rises with the concentration, he explained. And high viscosities can cause extravasation, which can harm local tissue, if not properly treated.
A good way to go, Molvin said, is to adjust the protocol to use a lower concentration of the contrast agent: “By doing so, the technologist can use the exact same injection parameters — flow rate, injection volume and injection duration — then just optimize the concentration based on the patient’s renal function.”
For example, at Stanford, a contrast medium with 300 concentration may be used instead of one with a 370 concentration, if eGFR (estimated glomerular filtration rate) indicates stage 3B chronic kidney disease, Molvin noted.
Working with Machines
People — working effectively with power injectors — are indispensible to insuring the safety of patients undergoing a contrast-enhanced CT. “There are no benefits to the patient from a nondiagnostic exam — only harm,” he said.
This harm may be physical, financial or both — physical from the unnecessary exposure of the patient to radiation; financial from the cost of the valueless exam. “A good CT scan with optimal enhancement can save the patient from having additional tests,” Molvin said.
In some cases lengthy delays could lead to death. This might happen, for example, if the CT prescribed for a patient suspected of pulmonary embolism were nondiagnostic – and the final diagnosis was delayed for too long.
“In CT you might have one shot to get it right and the contrast could make or break your study,” he said. “There (can be) incredible cost to the patient if you cut corners and don’t take good pictures.”
Greg Freiherr is a contributing editor to ITN. Over the past three decades, he has served as business and technology editor for publications in medical imaging, as well as consulted for vendors, professional organizations, academia, and financial institutions.
Editor’s Note: This is the first blog in a series titled Using Contrast Media. The next blog will focus on how innovation can help protect patients.
Related content:
Computed Tomography Angiography: A Review and Technical Update
TH-C-18A-08: A Management Tool for CT Dose Monitoring, Analysis, and Protocol Review


 March 06, 2026
March 06, 2026 









