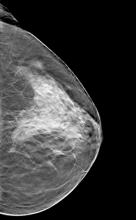
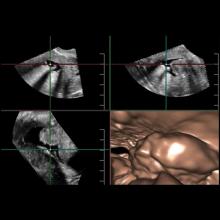
Breast density notification is becoming a reality in many states across the nation by virtue of legislation. A detailed review of breast density is beyond the scope of this article, but there are a few points that bear emphasis.
If you enjoy this content, please share it with a colleague
- Read more about Breast Density Assessment
- Log in or register to post comments