August 12, 2009 – Researchers at the Georgia Institute of Technology, collaborating with pediatric cardiologists and surgeons at The Children's Hospital of Philadelphia, have developed a tool for virtual surgery that allows heart surgeons to view the predicted effects of different surgical approaches by manipulating 3D cardiac MRIs of a patient's specific anatomy.
Physicians can compare how alternative approaches affect blood flow and expected outcomes and can select the best approach for each patient before entering the operating room.
"This tool helps us to get the best result for each patient," said coauthor Mark A. Fogel, M.D., an associate professor of cardiology and radiology, and director of cardiac MRI at The Children's Hospital of Philadelphia. "The team can assess the different surgical options to achieve the best blood flow and the optimum mixture of blood, so we can maximize the heart's energy efficiency."
In the August issue of the Journal of the American College of Cardiology: Cardiovascular Imaging, the researchers describe the surgical planning methodology, detailing how the tool helped them to plan the surgery of a four-year-old girl who was born with just one functional ventricle, or pumping chamber, instead of two.
Two in every 1,000 babies in the United States are born with this type of single ventricle heart defect. These children typically suffer from low levels of oxygen in their tissues because their oxygen-rich and oxygen-poor blood mix in their one functional ventricle before being redistributed to their lungs and body.
To correct this, the children undergo a series of three open-heart surgeries, called the staged Fontan reconstruction, to reshape the circulation in a way that allows oxygen-poor blood to flow from the limbs directly to the lungs without going through the heart. While these vascular modifications can eliminate blood mixing and restore normal oxygenation levels, surgeons and cardiologists must ensure that the lungs will receive proper amounts of blood and nutrients after the surgery so that normal development occurs.
"Preoperatively determining the Fontan configuration that will achieve balanced blood flow to the lungs is very difficult and the wide variety and complexity of patients' anatomies requires an approach that is very specific and personalized," said Ajit Yoganathan, Ph.D., regents' professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University. "With our surgical planning framework, the physicians gain a better understanding of each child's unique heart defect, thus improving the surgery outcome and recovery time."
The patient described in this paper, Amanda Mayer, age 4, of Staten Island, N.Y., had previously undergone all three stages of the Fontan procedure at The Children's Hospital of Philadelphia, but developed severe complications. Her oxygen saturation was very low, at only 72 percent, compared to normal levels of at least 95 percent. This is an indication of the possibility of abnormal connections between the veins and arteries in one of her lungs. Normally, the liver releases hormonal factors that prevent these abnormal connections, so the presence of the malformations indicated a low supply of hepatic blood to the lung.
To improve the distribution of these hormonal factors to both lungs, the surgeons needed to reoperate and reconfigure the patient's cardiovascular anatomy. Georgia Tech's surgical planning framework helped Thomas L. Spray, M.D., chief of the division of cardiothoracic surgery at Children's Hospital, to determine the optimal surgical option.
"MRI acquires images of the child's heart without using radiation," said Dr. Spray. "Then we use the computerized technology to model different connections to simulate optimum blood flow characteristics, before we perform the surgery."
The image-based surgical planning consisted of five major steps: acquiring magnetic resonance images of the child's heart at different times in the cardiac cycle, modeling the preoperative heart anatomy and blood flow, performing virtual surgeries, using computational fluid dynamics to model the proposed postoperative flow, and measuring the distribution of liver-derived hormonal factors and other clinically relevant parameters as feedback to the surgeon.
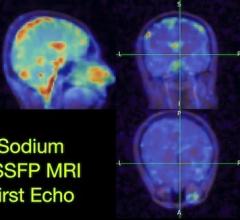
Dr. Fogel collected three different types of magnetic resonance images, and Yoganathan, along with graduate students Kartik Sundareswaran and Diane de Zelicourt, generated a three-dimensional model of the child's cardiovascular anatomy. From the model they reconstructed the three-dimensional pre-operative flow fields to understand the underlying causes of the malformations.
For this particular patient, the team saw a highly uneven flow distribution -- the left lung was receiving about 70 percent of the blood pumped out by the heart, but only five percent of the hepatic blood. Both observations suggested left lung malformations, but closer examination of the flow structures in that particular patient revealed that the competition between different vessels at the center of the original Fontan connection effectively forced all hepatic factors into the right lung even though a vast majority of total cardiac output went to the left lung.
To facilitate the design of the surgical options that would correct this problem, Jarek Rossignac, Ph.D., a professor in Georgia Tech's School of Interactive Computing, developed Surgem, an interactive geometric modeling environment that allowed the surgeon to use both hands and natural gestures in three-dimensions to grab, pull, twist and bend a 3D computer representation of the patient's anatomy. After analyzing the three-dimensional reconstruction of the failing cardiovascular geometry, the team considered three surgical options.
The research team then performed computational fluid dynamics simulations on all three options to investigate for each how well blood would flow to the lungs and the amount of energy required to drive blood through each connection design. These measures of clinical performance allowed the cardiologists and surgeons to conduct a risk/benefit analysis, which also included factors such as difficulty of completion and potential complications.
Of the three choices, Spray favored the option that showed a slightly higher energy cost but exhibited the best performance with regards to hepatic factor distribution to the left and right lungs. Five months after the surgery, Mayer showed a dramatic improvement in her overall clinical condition and oxygen saturation levels, which increased from 72 to 94 percent. Mayer is breathing easier and is now able to play actively like other children, according to her cardiologist, Donald Putman, M.D., of Staten Island, N.Y.
"The ability to perform this work is a team effort," Dr. Fogel added. "State-of-the-art three-dimensional cardiac MRI married to modern biomedical engineering and applied anatomy and physiology enabled this approach. With the advanced pediatric cardiothoracic surgery we have here at The Children's Hospital of Philadelphia, patients can benefit from this new method."
For more information: www.chop.edu


 February 13, 2026
February 13, 2026