October 18, 2017 — Magnetic resonance imaging (MRI)-based measurements of the functional connections in the brain can help predict long-term recovery in patients who suffer neurological disability after cardiac arrest, according to a clinical study appearing online in the journal Radiology.
Cardiac arrest, or abrupt loss in heart function, is a common and often deadly occurrence that affects hundreds of thousands of people every year in the United States alone, according to the American Heart Association. Many patients who survive end up with severe neurological disabilities, as the temporary loss of oxygenated blood flow to the brain can result in widespread neuronal cell death.
“Current methods to predict future levels of function for these survivors have limited accuracy,” said study lead author Robert D. Stevens, M.D., from Johns Hopkins University School of Medicine in Baltimore. “We need better methods to help clinicians understand the magnitude of these injuries and make more accurate predictions on recovery, thereby enabling more informed decision-making.”
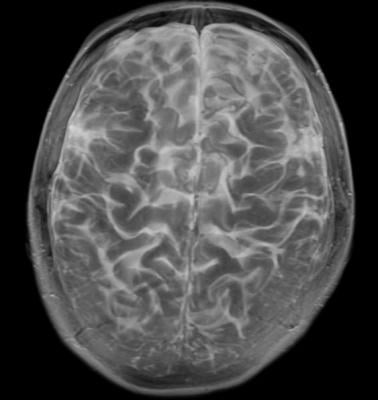
For the study, Stevens and colleagues used advanced MRI neuro imaging techniques like diffusion tensor imaging and resting-state functional MRI (fMRI) to focus on the brain’s large-scale functional integration. This “network of networks,” or connectome, represents the ensemble of different neuronal populations in the brain that work together to perform tasks.
The researchers assessed the brain’s functional connectivity in 46 patients who were in a coma following cardiac arrest. The imaging, performed within two weeks of cardiac arrest, included studies of brain structure and function. Functional imaging focused on four well-characterized networks in the brain, including the default mode network, which is active when a person is not engaged in a specific task, and the salience network, a collection of brain regions that select which stimuli are deserving of our attention.
One year after the patients’ cardiac arrests, the researchers assessed the patients with the Cerebral Performance Category Scale, a commonly used measure of neurological function following cardiac arrest. Eleven patients had favorable outcomes. Functional connectivity was stronger in those who achieved higher levels of independence at one year compared with those who were heavily dependent. The changes in functional connectivity between networks predicted outcomes with greater accuracy than any of the MRI structural measures tested.
“This is game-changing information about what happens in the brains of people who suffer cardiac arrest,” Stevens said. “We realize that network architectures can be selectively disrupted in this setting.”
A key predictor of outcomes was the interaction between the brain’s default mode and salience networks. These two networks are normally anti-correlated, meaning that as the default mode network becomes more active, activity is reduced in the salience network, and vice versa. When researchers compared the brain imaging results of patients who had favorable outcomes with those who did not, they noticed a stark difference.
“Anti-correlation was preserved in patients who recovered and abolished in those who did not,” Stevens said. “Relative preservation of this anti-correlation was the most robust signal of a favorable outcome.”
The results indicate that connectivity measures could be early markers of long-term recovery potential in patients with cardiac arrest-related brain damage, the researchers said.
While researchers don’t expect connectome analysis with MRI to be the single “magic bullet” solution to predicting outcomes, it could increase the confidence that clinicians have in communicating with patients’ families in the wake of cardiac arrest. Additionally, fMRI could aid in the development of therapeutic interventions for neurologically disabled patients.
“Connectome studies have the potential to change not only outcome prediction, but to guide treatment as well,” Stevens said.
For more information: www.pubs.rsna.org/journal/radiology


 February 13, 2026
February 13, 2026 









