May 30, 2018 — An updated American Cancer Society guideline says colorectal cancer screening should begin at age 45 for people at average risk. The recommendation is based in part on data showing rates of colorectal cancer are increasing in young and middle-aged populations.
The new recommended starting age is based on:
- Colorectal cancer (CRC) incidence rates;
- Results from microsimulation modeling that demonstrate a favorable benefit-to-burden balance of screening beginning at age 45; and
- The expectation that screening will perform similarly in adults ages 45 to 49 as it does in adults for whom screening is currently recommended (50 and older).
The updated recommendations are published early online in CA: A Cancer Journal for Clinicians, a peer-reviewed journal of the American Cancer Society.
The American Cancer Society recommends:
- Adults ages 45 and older with an average risk of colorectal cancer undergo regular screening with either a high-sensitivity stool-based test or a structural (visual) exam, depending on patient preference and test availability.
- The change in starting age is designated as a “qualified recommendation,” because there is less direct evidence of the balance of benefits and harms, or patients’ values and preferences, related to CRC screening in adults aged 45-49 since most studies have only included adults aged 50+. The recommendation for regular screening in adults aged 50 years and older is designated as a “strong recommendation,” on the basis of the greater strength of the evidence and the judgment of the overall benefit.
- As a part of the screening process, all positive results on non-colonoscopy screening tests should be followed up with timely colonoscopy.
- Average-risk adults in good health with a life expectancy of greater than 10 years should continue colorectal cancer screening through age 75. Clinicians should individualize colorectal cancer screening decisions for individuals ages 76 through 85, based on patient preferences, life expectancy, health status, and prior screening history. Clinicians should discourage individuals over age 85 from continuing colorectal cancer screening.
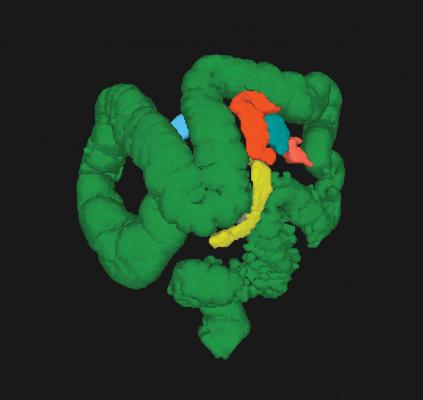
The recommended options for colorectal cancer screening are: fecal immunochemical test (FIT) annually; high sensitivity guaiac-based fecal occult blood test (HSgFOBT) annually; multi-target stool DNA test (mt-sDNA) every three years; colonoscopy every 10 years; computed tomography colonography (CTC) every five years; and flexible sigmoidoscopy (FS) every five years.
The new guideline does not prioritize among screening test options. Given the evidence that adults vary in their test preferences, the guidelines development committee emphasized that screening rates could be improved by endorsing the full range of tests without preference. The American Cancer Society has developed new materials to facilitate conversations between clinicians and patients to help patients decide which test is best for them.
“When we began this guideline update, we were initially focused on whether screening should begin earlier in racial subgroups with higher colorectal cancer incidence, which some organizations already recommend,” said Richard C. Wender, M.D., chief cancer control officer for the American Cancer Society. “But as we saw data pointing to a persistent trend of increasing colorectal cancer incidence in younger adults, including American Cancer Society research that indicated this effect would carry forward with increasing age, we decided to reevaluate the age to initiate screening in all U.S. adults.”
Colorectal cancer incidence has declined steadily over the past two decades in people 55 and over due to screening that results in removal of polyps, as well as changes in exposure to risk factors. But there has been a 51 percent increase in colorectal cancer among those under age 50 since 1994. Death rates in this age group have also begun to rise in recent years, indicating that increased incidence rates do not appear to be solely the result of increased use of colonoscopy. A recent analysis found that adults born around 1990 have twice the risk of colon cancer and four times the risk of rectal cancer compared with adults born around 1950, who have the lowest risk.
While the colorectal cancer incidence rate among adults 45 to 49 is lower than it is among adults 50 to 54 (31.4 versus 58.4 per 100,000), the higher rate in the 50-54 age group is partially influenced by the uptake of screening at age 50, which leads to an increase in the incidence rate due to detection of prevalent cancers before symptoms arise. Since adults in their 40s are far less likely to be screened than those in their 50s (17.8 percent vsersus 45.3 percent), the true underlying risk in adults aged 45-49 years is likely closer to the risk in adults ages 50 to 54 than the most recent age-specific rates would suggest. Importantly, studies suggest the younger age cohorts will continue to carry the elevated risk forward with them as they age.
Organizations have increasingly relied on modeling to evaluate alternative CRC screening strategies, including variations in the age to start and stop screening. Two of three microsimulation models conducted for the 2016 U.S. Preventive Services Task Force (USPSTF) screening recommendations suggested that starting colonoscopy screening with an interval of 15 years at age 45 vs age 50 provided a slightly more favorable balance between the benefits and burden of screening. However, the USPSTF elected not to recommend the younger starting age in 2016. The task force judged the estimated additional benefit to be “modest,” and also noted that one of the three models did not corroborate the additional benefit and there was a lack of empirical evidence to support the change.
A new modeling study commissioned by ACS for this review extended these analyses by incorporating more recent studies of the rising incidence trends in younger adults. The study showed that multiple screening strategies beginning at age 45, including colonoscopy at the conventional 10-year interval, had a more favorable benefit to burden ratio with more life-years gained compared with starting screening at age 50.
“One of the most significant and disturbing developments in CRC is the marked increase in CRC incidence – particularly rectal cancer --among younger individuals,” concluded the authors. “While the causes of this increase are not understood, it has been observed in all adult age groups below the age when screening has historically been offered, and is contributing significantly to the burden of suffering imposed by premature CRC mortality. Incorporating this epidemiological shift into contemporary modeling of CRC screening demonstrated that the benefit-burden balance is improved by lowering the age to initiate CRC screening to 45 years. Lowering the starting age is expected to benefit not only the segments of the population who suffer disproportionately from CRC – blacks, Alaska Natives and American Indians – but also those individuals otherwise considered to be at average risk. Moreover, epidemiological trends in cohorts as young as those born in 1990 suggest that the higher risk of developing CRC will be a persistent concern for decades to come.”
The new ACS guidelines received the full endorsement of the Colorectal Cancer Alliance (CCA), the oldest and largest colorectal cancer nonprofit organization in the U.S. “By 2030, 10.9 percent of all colon cancers and 22.9 percent of all rectal cancers will be diagnosed in patients younger than age 50,” said Colorectal Cancer Alliance CEO Michael Sapienza. “Together we must defy and redefine the odds...If this new guideline is adopted, lives will be saved.”
Sapienza also announced that the CCA plans to invest $10 million in critical research by 2021, which will include “learning why we are seeing an increase in young-onset colorectal cancer, doubling the number of constituents we serve, and saving 100,000 lives by 2026 through increased screening.”
The full ACS guideline can be read here.
For more information: www.cancer.org
Related Colorectal Cancer Screening Content
The Future of CT Colonography Screening
U.S. Healthcare Facilities Have Capacity to Meet Colorectal Cancer Screening Goals
USPSTF Approves CT Colonoscopy for Colorectal Cancer Screening


 March 03, 2026
March 03, 2026 









