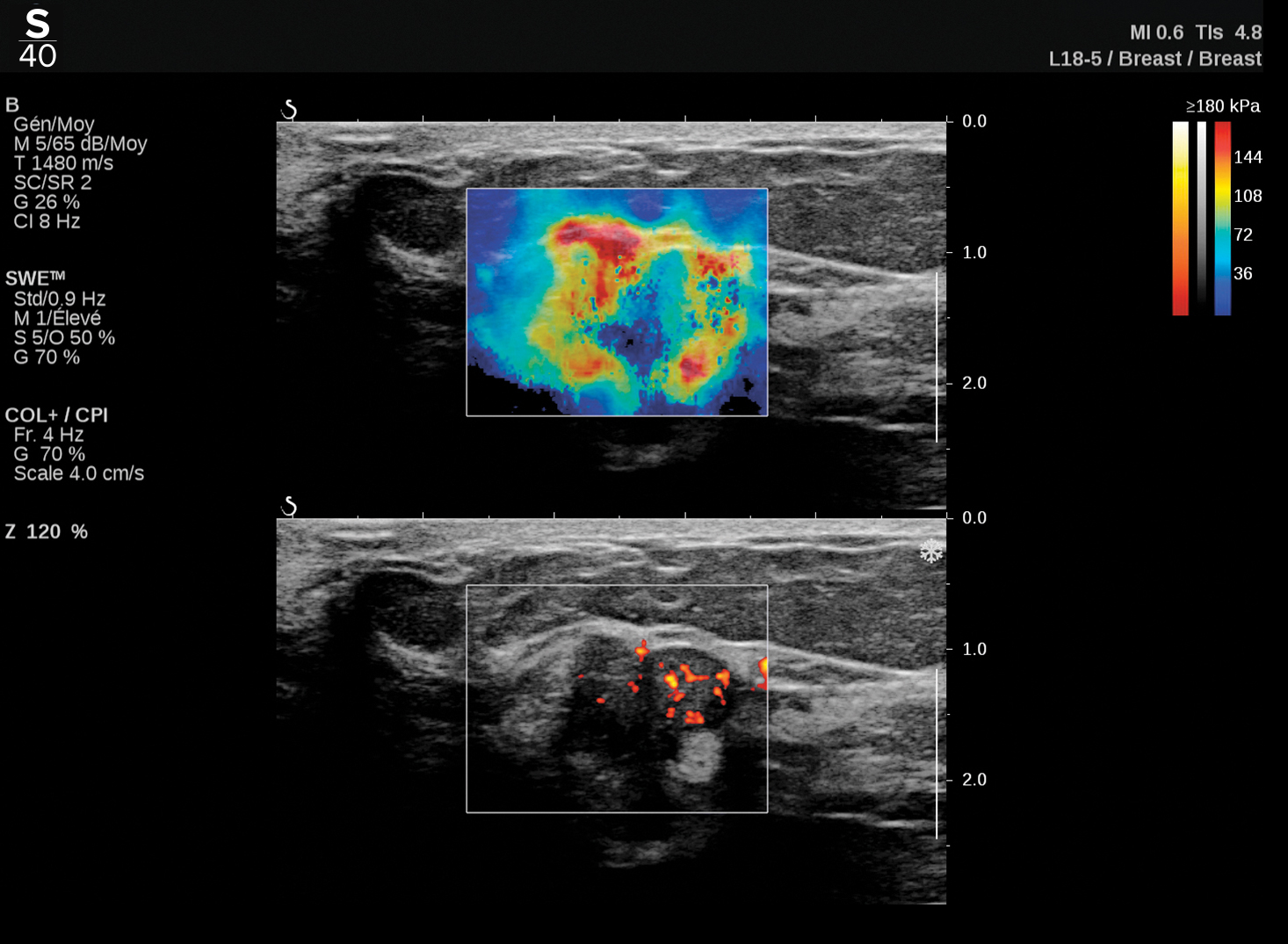
This is an example of TriVu ultrasound imaging on a breast, designed to help increase efficiency and diagnostic accuracy in any practice. Image courtesy of Hologic.
The breast ultrasound market is seeing growth, driven largely by the proliferation of recent legislation aimed at addressing the unique challenges of imaging dense breast patients. Today, many governmental screening programs encourage the use of breast ultrasound for women with dense breast tissue, largely because ultrasound can differentiate between normal dense tissue and lesions better than traditional 2-D mammography. As the breast ultrasound market continues to grow, its impact on the breast care continuum naturally rises in tandem.
Amidst this market expansion, it becomes increasingly important to understand today’s breast ultrasound trends, as they hint at where the industry is headed in the future and predict what we can expect to see in the coming years.
The Rise of Shear Wave Elastography
Although ultrasound receives exceptional marks for sensitivity, its specificity has long been a shortcoming of the modality with notable opportunities for improvement. In response, shear wave elastography has been growing in popularity thanks to its ability to help increase clinicians’ diagnostic accuracy and subsequently impact specificity.
Although some professionals gave shear wave elastography a somewhat lackluster welcoming in the technology’s infancy due to uncertainty surrounding its usefulness, the latest generations of shear wave elastography have reversed this perception for many thanks to its notable benefits and improvements, including the clear diagnostic value the technology imparts. Today, the added value of shear wave elastography is recognized by major scientific societies1 in ultrasound, and it is backed by a long track record of scientific research with countless breast imaging publications. Shear wave elastography has been found to aid in the diagnostic work up of breast lesions, which positively impacts patient management.2 It also helps with targeting lesions during ultrasound-guided biopsy,3 and it contributes to an accurate lesion size measurement.4 In addition, the technology plays a role in prognostics and monitoring of breast cancer patients during and after neoadjuvant chemotherapy.5
Recently, 3-D shear wave elastography was introduced to the field, further enhancing the technology by providing the ability to visualize breast tissue in any plane of 3-D volume and allowing readers to preview information on the elasticity distribution inside and around the lesion.
Looking to the future, there will likely be more widespread adoption of the technology as ultrasound users increasingly recognize the added diagnostic value of evaluating tissue stiffness alongside b-mode and other traditional ultrasound imaging modes, particularly for the purposes of more confidently downgrading lesions to avoid unnecessary biopsies.
The Expanded Role of Automation and AI
There are countless opportunities to improve the efficiency and workflow of ultrasound exams, and there is demand for solutions to address these challenges. In fact, in a recent survey, 90 percent of ultrasound users agreed that workflow efficiency is an important consideration when purchasing a new ultrasound system.6 Given this environment, it’s evident there will be an uptick in ultrasound innovations striving to optimize workflow and cutback on time-consuming inefficiencies of the ultrasound exam.
The reality is that a lot of the current ultrasound workflow could potentially be augmented — or even completely supplanted — by technology, particularly with future artificial intelligence (AI) integrations. This includes tasks such as documentation, annotation and time spent looking for lesions on images, which could readily be addressed with AI-based tools that allow for pre-selection of relevant images, automatic or semi-automatic measurements, enhanced labeling and reporting, and beyond.
Furthermore, variability in inter-reader breast lesion assessment with ultrasound, growing workloads and limited staff continue to be significant challenges for the breast imaging community. AI and machine learning based tools can empower physicians and sonographers to overcome these challenges. They are expected to help improve diagnostic accuracy by increasing both sensitivity and specificity, increase diagnostic confidence with decision-making support tools, increase reproducibility by addressing inter-reader variability and decreasing operator dependency, and improve the overall user experience.
There will clearly be a significant role for automation and AI to play in the future of ultrasound, and this is being fast-tracked by the COVID-19 pandemic. In the short term, the pandemic has accelerated the development of AI software across the healthcare sector overall and highlighted the need for further investment in AI-based medical imaging and machine learning tools for patient screening, triage and monitoring. In addition, the pandemic has increased investment in technology for faster response time and more ubiquitous use of AI.
With the increased focus on overcoming barriers to entry, COVID-19 could become an accelerant to long-lasting adoption of AI in the healthcare sector, and this will naturally parlay into the breast ultrasound industry, which is ripe with opportunities for AI to make a definitive impact on workflow efficiencies and outcomes.
The Reduction of Repetitive Stress Injuries
Finally, a lingering challenge associated with ultrasound imaging is the continued prevalence of repetitive stress injuries and musculoskeletal disorders associated with scanning. There is a clear need for targeted solutions, as research suggests approximately 80-90.5 percent of sonographers are scanning in pain.7,8,9
Thankfully for sonographers, we are already seeing a rise in technology innovations pointed toward enhancing ergonomics through thoughtful design considerations. An example of which is a movement away from the traditional trackball used by many ultrasound systems toward a touchpad design that aims to reduce users’ movements and mimic the intuitive functionality of the ubiquitous smartphones permeating today’s society. Another example is design adjustments to the transducers themselves, which are becoming lighter and more ergonomic than prior generations.
We expect ergonomic design considerations will continue to rise in prevalence in future ultrasound technology, particularly because ultrasound users have rallied behind the improvements. In one study, 9 in 10 ultrasound users agreed that ergonomics is an important consideration when making a new ultrasound system purchasing decision.10
Although one cannot know definitively what the future of breast ultrasound holds in the next 10+ years, the challenges and trends of today provide a roadmap for where we are headed and what advancements may help us get there. What we do know with certainty is that ultrasound will remain an essential tool in a breast imager’s arsenal for managing breast health across the care continuum. Medical technology manufacturers working in close unison with clinicians, sonographers and patients will be the most successful at driving these innovations and setting the tone for the future of breast ultrasound.

Jennifer Meade is the President of Hologic’s Breast and Skeletal Health Division and has been a part of the company since 2006. In her role, she is committed to continuing to drive innovation across the breast care continuum and investing in the Company’s people to ultimately drive improved outcomes for patients around the globe.
References:
1. ACR BI RADS: Ultrasound (2015), KSUM Guidelines for breast elastography (2014), EFSUMB (2013) and WFUMB Guidelines
2. Shearwave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Berg WA et al. Radiology. 2012 Feb;262(2):4 35 49.
3. Addition of shear wave elastography during second look MR imaging directed breast US: effect on lesion detection and biopsy targeting. Plecha DM, Pham RM, Klein N, Coffey A, Sattar A, Marshall H. Radiology. 2014 Sep;272(3):657 64.
4. Shear-wave elastography contributes to accurate tumour size estimation when assessing small breast cancers. Mullen R et al. Clin Radiol. 2014 Dec;69(12):1259-63
5. Comparison of strain and shear-wave ultrasonic elastography in predicting the pathological response to neoadjuvant chemotherapy in breast cancers. Ma Y et al. Eur Radiol. 2017 Jun;27(6):2282-2291. I Shear-Wave Elastography for the Detection of Residual Breast Cancer After Neoadjuvant Chemotherapy. Lee SH et al. Ann Surg Oncol. 2015 Dec;22 Suppl 3:S376-84.
6. An online survey administered in the U.S. among 210 individuals who identified their job title as radiologist, sonographer or ultrasound technologist, and who had one (1) or more years of ultrasound experience (2021).
7. Evans K, Roll S, Baker J. Work-related musculoskeletal disorders (WRMSD) among registered diagnostic medical sonographers and vascular technologists. A representative sample. J Diagn Med Sonog 2009; 25: 287–99.
8. Pike I, Russo A, Berkowitz J, et al. The prevalence of musculoskeletal disorders among diagnostic medical sonographers. J Diagn Med Sonog 1997; 13: 219–27.
9. Harrison G, Harris A. Work-related musculoskeletal disorders in ultrasound: Can you reduce risk? Ultrasound. 2015;23(4):224-230. doi:10.1177/1742271X15593575
10. An online survey administered in the U.S. among 210 individuals who identified their job title as radiologist, sonographer or ultrasound technologist, and who had one (1) or more years of ultrasound experience (2021).
Related Breast Ultrasound Content:
Artificial Intelligence Improves Accuracy of Breast Ultrasound Diagnoses
Routine Screening Return for BI-RADS 3 Lesions on Supplemental Automated Whole-Breast Ultrasound



 February 13, 2026
February 13, 2026