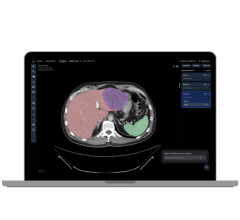
3-D MSOT rendering of a basal cell carcinoma. Image courtesy of Singapore BioImaging Consortium
November 20 2017 — Scientists and clinicians from Singapore and Germany have successfully used multispectral optoacoustic tomography (MSOT) to achieve accurate, real-time 3-D imaging of non-melanoma skin cancer tumors. This imaging technique uses a combination of light pulses and ultrasound waves to form 3-D images that are precise in dimensions and depth.
This is a breakthrough in non-invasive skin imaging, as this technique allows for the imaging of tumors that are deep below the skin (up to 30mm below the skin surface) and provides high-resolution results with clear differentiation of the various tissues. Current imaging techniques can only image tumors no deeper than 3mm below the skin, and in some cases produce results that do not accurately show the tumor in contrast to other tissues such as fat.
The team that discovered this comprised of scientists from A*STAR’s Singapore Bioimaging Consortium (SBIC) and the Technical University of Munich (TUM) in Germany, and clinicians from the National Skin Centre (NSC) and the Skin Research Institute of Singapore (SRIS) who ran the patient tests. The findings were published in Elsevier’s Photoacoustics journal and were highlighted as a promising first-in-man clinical study during the recent 2017 World Molecular Imaging Congress, Sept. 13-16 in Philadelphia.
Due to limitations in existing skin imaging tools, non-melanoma skin cancer tumors cannot be imaged clearly pre-surgery, often resulting in either excess or incomplete removal of the cancerous tissue. Through the use of MSOT, the team found a way to overcome these limitations. This technique produces images by sending out light pulses of varying wavelengths that tissues absorb, expand and emit ultrasound waves which converge to form images. Since different tissues absorb different wavelengths of light, varying the wavelength will reveal which tissues are present. The high-resolution images produced using MSOT allow clinicians and doctors to view the lesions’ dimensions, depth and the underlying vascular tissue. Such information is critical in identifying cancer and the level of aggression of a tumor.
One of the main techniques for treating skin cancer is Mohs micrographic surgery, which involves the removal of one layer of tissue at a time, which is then studied under a microscope to ensure that there are no more cancer cells. Compared to this time-consuming procedure, the application of MSOT pre-surgery could enable much shorter surgical procedures due to the highly accurate identification of tumor size, depth and contrast versus surrounding tissues.
“This first-in-man study has successfully demonstrated that the use of MSOT can vastly improve the accuracy of the diagnosis and effectiveness of the treatment of non-melanoma skin cancer,” said Prof. Malini Olivo, director of biophotonics and head of the Laboratory of Bio-Optical Imaging at SBIC, who led the study.
Prof. Steven Thng, executive director of SRIS and Senior Consultant of NSC, who co-led the study, said: “The ability to image skin cancer in 3D in-vivo will prove to be the disruptive technology for skin cancer management in the future. This will change the paradigm of how skin cancer will be managed as dermatosurgeons will now be able to visualise the tumor before surgery and individualize surgery based on tumor characteristics and size. This will minimize relapse rates due to inadequate surgery, and reduce unnecessary scarring because of oversampling.”
In Singapore, skin cancer is among the top 10 most common cancers in both men and women. The two most common types of skin cancer in Singapore are basal cell carcinoma and squamous cell carcinoma, both non-melanoma skin cancers.1
For more information: www.journals.elsevier.com/photoacoustice
Reference
1. Prevalence of skin cancer in Singapore: https://www.nccs.com.sg/PatientCare/WhatisCancer/TypesofCancer/Pages/skin- cancer.aspx?p=/PatientCare


 February 05, 2026
February 05, 2026