A prostate MRI showing benign prostatic hyperplasia (BPH).
Radiologists play a key role in the cancer care continuum after the initial diagnosis of prostate cancer. This includes regular imaging assessments to monitor growth, and tracking tumor changes to measure the effectiveness of various therapies. For the radiologist evaluating prostate cancer, it is key to first determine the severity of the disease, which determines whether the patient will be monitored over the course of several years, or if immediate treatment is required.
“The greatest challenge is to distinguish patients who need aggressive treatment and those who are low-risk,” said Hedvig Hricak, M.D., Ph.D., chair of the Department of Radiology at Memorial Sloan-Kettering Cancer Center, New York. She spoke on prostate assessment at the 2014 Radiological Society of North America (RSNA) meeting in December. Aggressive prostate cancer is treated with radical prostatectomy (RP), radiation therapy (RT), brachytherapy or cryotherapy. All of these require post-treatment monitoring to ensure the therapy is working and see if new cancer activity is present, she explained.
Hricak said contrast-enhanced magnetic resonance imaging (MRI) has emerged as the current standard for assessing local recurrence of prostate cancer after RP or RT. She explained that early detection of local recurrence is important to allow potentially curative salvage therapy. Prostate biopsies are usually ordered when prostate-specific antigen (PSA) levels reach 2.5 ng/mL or higher. There are no PSA levels that determine when a prostate MRI should be ordered, however she said the earlier the better for diagnosis and for detecting recurrence. “You should not wait for clinical symptoms before ordering an MRI,” Hricak said. “There also is definitely an emerging acceptance of MRI in newly diagnosed PSA biochemical recurrence.”
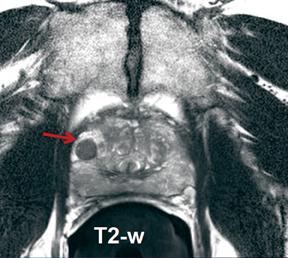
It is important to know how MRI protocols for detecting local recurrence should be adjusted depending on the prior treatment and the questions being asked. Hricak offered several examples. After RT, T2-weighted MRI is limited due to post-radiation effects on the prostate such as glandular shrinkage, loss of normal zonal anatomy and reduced contrast between cancer and normal tissue caused by glandular atrophy and fibrosis.
She said MRI should include both T2-weighted and diffusion-weighted imaging (DWI) sequences. A recent study suggests that in most patients, dynamic contrast-enhanced (DCE) MRI could be omitted after RT without lowering diagnostic performance. She said this also eliminates the risks and costs associated with the use of contrast.
If salvage treatment is an option after RT, MRI offers locoregional staging. Post-RT MRI can evaluate the length of the urethra and may show urethral shortening (which has been associated with incontinence after primary RP), decreased urethral margin definition and other tissue changes that could conceivably affect treatment selection and planning.
After surgery, in addition to DWI, the use of DCE/MRI is essential. Hricak explained that it can show small lesions and differentiate a tumor from scarring. MRI may help to determine whether post-RP local recurrence is amenable to salvage RT, and may aid RT planning.
The Role of Nuclear Imaging
Assessment of prostate cancer recurrence after emerging focal therapies remains problematic, since methods for reliably differentiating necrosis or scarring from tumors are lacking. In the future, Hricak said PET/CT with targeted tracers may be able to address this need. PET/CT and bone scanning are valuable in the search for nodal and osseous metastases, she explained, adding that the implementation of clinical PET/MRI and the use of new tracers will likely open new horizons in the assessment of recurrence.
Hricak said nuclear imaging with PET/CT or PET/MRI also can help in evaluating prostate treatments, stating that nuclear scans can offer an attractive alternative to MRI for patients, since MRI requires use of an endorectal coil. “The patient is not going to keep coming back if you always use an endorectal coil,” she explained.
New MRI Imaging Techniques
Standard contrast MRI often misses tumors that do not significantly differ from surrounding healthy tissues with contrast. For this reason, diffusion MRI is being used at some centers to measure the diffusion of water in and around the prostate. Diffusion MRI is a standard technique for brain imaging. Cancer tissues are denser than healthy tissues, which limits the amount and mobility of water within them.
However, a big issue with diffusion MRI is that imaging can suffer from magnetic field artifacts that can distort the actual location of tumors by as much as 1.2 cm. This becomes an issue when surgeons are trying to determine if a tumor extends beyond the prostate and into adjacent nerve bundles.
The new approach, called restriction spectrum imaging-MRI, or RSI/MRI, corrects for magnetic field distortions and focuses on water diffusion within tumor cells. This has the ability to more accurately image and plot a tumor’s location and extent, said Nathan White, Ph.D., assistant project scientist at UC San Diego. He is the co-inventor of the RSI/MRI technique and co-author of a recently published paper on the subject in the journal Prostate Cancer and Prostatic Diseases.
“This new approach is a more reliable imaging technique for localizing tumors. It provides a better target for biopsies, especially for smaller tumors,” said Rebecca Rakow-Penner, M.D., Ph.D., a research resident in the Department of Radiology at UC San Diego and the study’s first author.
The technique is also valuable in surgical planning and image staging, said David S. Karow, M.D., Ph.D., assistant professor of radiology at UC San Diego and the study’s corresponding author. “Doctors at UC San Diego and UCLA now have a non-invasive imaging method to more accurately assess the local extent of the tumor and possibly predict the grade of the tumor, which can help them more precisely and effectively determine appropriate treatment,” he concluded.
Reference:
1 Rakow-Penner, R A , White, N S, Parsons, J K, et al. “Novel Technique for Characterizing Prostate Cancer Utilizing MRI Restriction Spectrum Imaging: Proof of Principle and Initial Clinical Experience with Extraprostatic Extension.” Prostate Cancer and Prostatic Diseases, Jan. 6, 2015.


 February 04, 2026
February 04, 2026 









