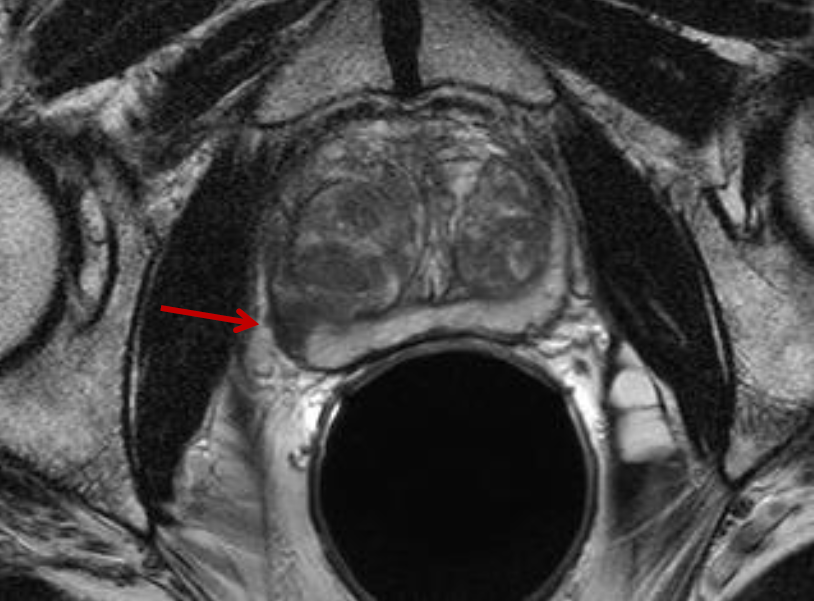
When prostate cancer makes a comeback, it becomes increasingly important to have exceptional imaging available to find all possible regions where cancer has spread to other parts of the body, or metastasized, in order to plan the best possible treatment. A relatively new imaging system that simultaneously combines positron emission tomography and magnetic resonance (PET/MR) demonstrates a higher capacity for mapping recurrent prostate cancer than the already high standard of integrated PET and computed tomography (PET/CT), say researchers presenting a study at the Society of Nuclear Medicine and Molecular Imaging’s 2013 Annual Meeting.
PET/MR provides superb soft tissue contrast with its MR component, compared to PET/CT, which focuses more on structure and density imaging with CT. This study ushers PET/MR into the ring of clinical practice by exhibiting clear benefits for prostate cancer patients with metastatic tumors.
In this comparative study recurrent prostate cancer is imaged both with PET/MR and PET/CT with the molecular imaging agent C-11 choline, which was approved for this use by the U.S. Food and Drug Administration (FDA) last year. Choline is a naturally occurring B vitamin complex that is avidly bound by prostate cells upon injection, even those that have traveled through the bloodstream and taken up residence to develop metastatic tumors elsewhere, which is especially likely in the lymph nodes and in bone.
“The combination of PET, here with C-11 choline, and functional MRI provides complementary information that increases diagnostic certainty with higher detection rates, especially for more precise localization of recurrence. This could help to better tailor specific therapy, e.g., radiation of the pelvis versus antihormonal therapy, for patients with metastatic prostate cancer,” said Matthias Eiber, MD, lead scientist for the study from TU Muenchen in Munich, Germany.
Methodology included a study population of 31 patients who had both PET/CT and PET/MR performed for restaging of recurrent prostate cancer with single injection of the imaging agent C-11 choline. PET/CT scans occurred about five minutes after injection, and PET/MR scans occurred about 51 minutes after injection. Scans were interpreted separately and all detected lesions were categorized according to suspected metastases as definitely, probably or indeterminately metastatic. Researchers discovered that PET/MR found more areas of metastases—17 in 12 different patients—when compared to PET/CT, which found 12 areas of metastases in eight subjects. PET/MR also found more lymph node metastases, 42 versus 39 areas of interest with PET/CT. The same held true for bone metastases, which were detected in 17 areas for five patients with PET/MR and 14 areas for four patients with PET/CT.
Simultaneous PET/MR is comparable to—if not more powerful than—PET/CT for recurrent prostate cancer. The only obvious challenge was a longer scan time than PET/CT, but it was found to be tolerable by patients undergoing PET/MR. PET/MR additionally offers considerably lower radiation exposure compared to PET/CT. As many of these patients often get a series of examinations in the course of their disease, despite their high average age, radiation protection could be another argument for the promotion of PET/MR. This molecular imaging technique can now be considered a conceivable alternative to PET/CT for restaging prostate metastases, especially when small local tumor recurrences are involved.
“In principle, whole-body integrated PET/MR is a technique that is officially commercially available; however, so far only a limited number of these scanners have been installed worldwide,” said Eiber. “Showing a concrete example of how combining PET and functional MR imaging benefits patients with metastatic prostate cancer could potentially motivate continued PET/MR research in this field.”
Scientific Paper 343: Matthias Eiber, Michael Souvatzoglou, Tobias Maurer, Sibylle Ziegler, Ernst Rummeny, Markus Schwaiger, Ambros Beer, Radiology, TU Muenchen, Munich, Germany; Nuclear Medicine, TU Muenchen, Munich, Germany; Urology, TU Muenchen, Munich, Germany, “Initial experience in restaging of patients with recurrent prostate cancer: Comparison of 11C-Choline-PET/MR and 11C-Choline-PET/CT,” SNMMI’s 60th Annual Meeting, June 8–12, 2013, Vancouver, British Columbia.
For more information: www.snmmi.org


 February 11, 2026
February 11, 2026