December 7, 2010 – Positron emission tomography/computed tomography (PET/CT) could be a useful tool for predicting local recurrence in lung cancer patients treated with radiofrequency ablation (RFA). Supporting data from a study was published in the December issue of The Journal of Nuclear Medicine.
RFA, which uses localized thermal energy to kill cancer cells, is increasingly used as an alternative treatment for patients unable to undergo surgery or other therapies to treat lung cancer.
"This study reinforces the utility of 18F-FDG-PET imaging in cancer detection and follow-up while also providing new insight into factors that can be used for earlier prediction of recurrence after radiofrequency ablation of lung tumors," said Amit Singnurkar, M.D., FRCPC, assistant professor of radiology and medicine at McMaster University and lead author of the study. Singnurkar was previously a nuclear oncology fellow at Memorial Sloan-Kettering Cancer Center, where the majority of the study was conducted.
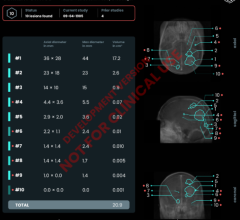
The five-year study followed 68 patients with 94 pulmonary lesions, including metastases and primary lung cancers. By reviewing 18F-FDG PET/CT scans performed before and after RFA, researchers were able to determine several indicators that could help predict local recurrence. Among pre-RFA scans, lesion size and tumor type (primary or metastases) were factors in determining potential for local recurrence. Standardized uptake value (glucose metabolic activity) was also a factor in pre-RFA scans, although not independent of lesion size. PET/CT scans conducted after RFA indicated that 18F-FDG uptake patterns, size of ablation margins and standardized uptake value were parameters that could predict the likelihood of recurrence.
Information gleaned from the pre- and post-PET/CT scans can increase the accuracy of recurrence detection and allow earlier diagnosis. This ultimately can facilitate better management, leading to improved patient outcomes.
"Used correctly, molecular imaging can provide more accurate and earlier results than anatomic imaging alone," Singnurkar said. "Molecular imaging has the potential to detect and characterize disease earlier, at a point where it can be more amenable to therapy."
For more information: www.snm.org


 February 11, 2026
February 11, 2026