November 28, 2019 — Individuals with functional neurological disorder (FND) have symptoms not explained by traditional neurological conditions, including limb weakness, tremor, gait abnormalities, seizures and sensory deficits. New research led by investigators at Massachusetts General Hospital (MGH) and published in Psychological Medicine has uncovered pathways in the brain's white matter that may be altered in patients with FND. The findings advance current understanding of the mechanisms involved in this disease, and offer the possibility of identifying markers of the condition and patients' prognosis.
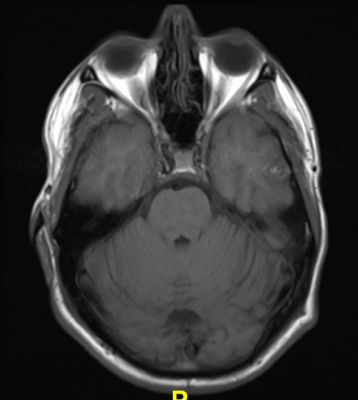
Because conventional tests such as clinical magnetic resonance imaging (MRI) brain scans and electroencephalograms (EEGs) are usually normal in patients with FND, there are currently no brain-based markers for this disorder and diagnoses are made using physical examination signs. More precise research-based imaging methods such as functional MRI and quantitative MRI have revealed several differences in the brains of some patients, including in gray matter regions. To look for any differences in the brain's white matter — which is composed of bundles of axons coated with protective myelin to help conduct nerve signals--investigators used a technique called diffusion tensor imaging (DTI), which measures the diffusion of water molecules.
The team used DTI to examine the brain white matter of 32 patients with FND and 36 healthy controls. Patients also provided information on the severity of their symptoms, the extent of the physical disability they experience, and the duration of their illness.
The researchers found that patient-reported impairments in physical health and illness duration were each associated with disruptions in white matter fibers within the stria terminalis/fornix, a pathway that is the principal output of the amygdala and hippocampus (brain areas that play roles in emotion/salience and learning/memory, respectively). This is notable given that several structural and functional neuroimaging studies have identified amygdalar and hippocampal abnormalities in patients with FND. Furthermore, reduced integrity within another pathway called the medial forebrain bundle also showed a relationship to patient-reported physical health impairments.
"The findings point to the potential importance of white matter pathways in the biology of FND," said lead author Ibai Diez, Ph.D., a senior research fellow in Neurology at MGH. "Our methodological approach here is another novelty. We conducted a set of network analyses that not only identifies patterns of white matter alterations, but also links specific patterns of white matter changes to cortical and subcortical brain areas."
Additional research is needed to determine the potential clinical relevance of the results. "Given that white matter disruptions in the stria terminalis/fornix and medial forebrain bundle related to patient-reported impairments in physical health and illness duration, future analyses should evaluate if these white matter profiles might be connected to specific clinical outcomes," said senior author David Perez, M.D., MMSc director of the MGH FND Clinical and Research Programs. "Our work also requires further clarification and replication in large sample future studies."


 March 03, 2026
March 03, 2026 









