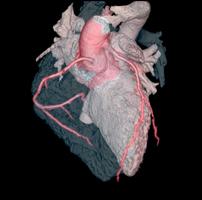
May 17, 2010 – When patients present with chest pain or other high-risk symptoms of heart problems, doctors increasingly rely on nuclear imaging and computed tomography (CT) to find evidence of heart disease. Results of these procedures can help guide life-saving prevention and treatment options.
However, despite their widespread use and efforts by the cardiac imaging community to reduce exposure to ionizing radiation, concerns over the potential cancer-causing effects of these diagnostic tests continue to dominate discussions. This may lead to imbalanced decision-making and heighten consumers’ fear of these tests, according to experts writing in the May 2010 issue of the Journal of the American College of Cardiology (JACC): Cardiovascular Imaging. This special issue explores the challenges of cardiac imaging, including how to effectively measure the radiation doses of different tests, as well as the lack of standard guidelines to evaluate risks and benefits of using such imaging tests.
“These tests are so widely applied now, the concern is that there is some potential of increased cancer risk associated with their use,” said Jagat Narula, M.D., Ph.D., division of cardiology, University of California, Irvine, and editor-in-chief of JACC: Cardiovascular Imaging. “The problem is that most estimates of radiation exposure stem from an extrapolation of studies on World War II Hiroshima survivors, and the radiation exposure from imaging tests may not necessarily be the same.”
As with anything in medicine, a careful analysis of the risks and benefits of cardiac imaging is warranted, and experts agree these tests should only be used when the clinical benefit is expected to exceed the potential harm.
“Because most patients undergoing cardiac imaging are symptomatic, the risk of heart disease is high, so the radiation risk is far less than the benefits gained,” said Leslee Shaw, Ph.D., professor of medicine, Emory University School of Medicine, Atlanta, Ga., and an author of the editorial. “If we can identify appropriate patients for testing, then we can provide more intensive treatment and the patient will likely have better outcomes. And, importantly, the radiation exposure is far less than the benefit gained from targeting treatment for heart disease.”
Of course, there are also some cases in which use of these tests may not afford the greatest benefit, according to authors. For example, the risk of exposing a 38-year-old woman of childbearing age who reports one episode of stabbing chest pain to radiation might be far greater than any benefit because her risk of coronary artery disease is so low. Other procedures, such as a routine treadmill test or electrocardiogram could be used to help rule out heart problems. In other cases, cardiac imaging can help rule out heart problems and redirect clinical care as needed.
“There has also been a tendency to play up the fears of radiation and we don’t want patients to be afraid of these tests,” Shaw explains, adding there have been some instances in which very sick patients refuse imaging procedures when the test would have been valuable in terms of their medical management and follow up. “We should encourage patients and doctors to talk about whether a test is needed, why it is being ordered and what it will show. Dialogue about the benefits of testing and the risks of radiation exposure is an essential part of the patient and physician decision making.”
Clinicians should educate patients about these tests and encourage them to be informed participants in decision making by asking themselves: “Am I going to gain more information by having this test, and am I willing to accept a small dose [of radiation] to find out?”
What is needed moving forward?
Recent advances in limiting radiation dose levels through quality imaging, technological advances and guidelines, such as the American College of Cardiology’s Appropriate Use Criteria, as well as keeping doses as low as reasonably appropriate (referred to as ALARA), are making a difference.
Authors stress there is a need for standardized measures for radiation exposure, long-term follow up of patients to better understand the safety profile in term of estimating cancer risk and cardiac benefits, especially among those with an elevated cancer risk, more comparative effectiveness studies that include radiation exposure as a primary safety endpoint, promotion of low-dose imaging protocols which can reduce radiation dose by more than half, new imaging techniques and equipment that reduce radiation exposure, and improved patient education programs about the risks and benefits of cardiac imaging.
For more information: www.acc.org


 February 13, 2026
February 13, 2026 









