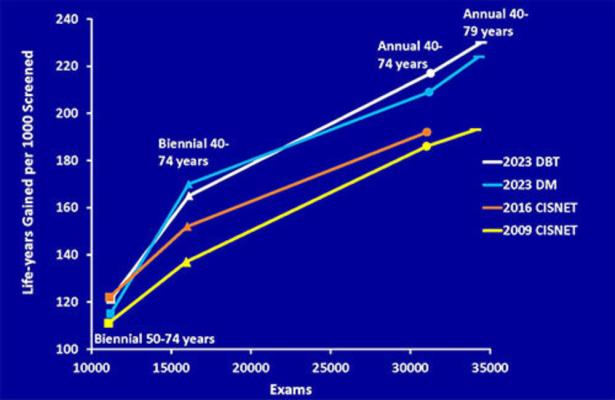
Figure 1. Line graph shows the estimates of life-years gained per 1,000 women screened versus screening examinations performed reported by the Cancer Intervention and Surveillance Modeling Network (CISNET) in 2009, 2016, and 2023 for the four protocols listed in Table 1, which are biennially ages 50–74 years (squares), biennially ages 40–74 years (triangles), annually ages 40–74 years (circles), and annually ages 40–79 years (bars). CISNET estimates for life-years gained have increased from 2009 to 2023 for each screening scenario as more recent data have been included in their models. Annual screening ages 40–79 years maximizes life-years gained. DBT = digital breast tomosynthesis, DM = digital mammography.
February 20, 2024 — Annual breast cancer screening beginning at age 40 and continuing to at least age 79 results in the highest reduction in mortality with minimal risks, according to a new study published today in Radiology, a journal of the Radiological Society of North America (RSNA).
Breast cancer is the second most common cause of cancer death for women in the U.S. Despite research demonstrating that consistent participation in screening mammography can reduce breast cancer deaths by 40%, only 50% or less of eligible women actually participate in annual screening.
“There is an ongoing debate over the recommendations for breast cancer screening, specifically about when to start and the frequency of screening,” said lead researcher Debra L. Monticciolo, M.D., professor of radiology at Dartmouth Geisel School of Medicine in Hanover, New Hampshire.
Dr. Monticciolo said a recommendation by the U.S. Preventive Services Task Force (USPSTF) in 2009 to screen every other year, or biennially, beginning at age 50 resulted in a nationwide decline in screening participation. The USPSTF drafted new recommendations in 2023, suggesting women participate in biennial screening between 40 and 74. The American College of Radiology, the Society of Breast Imaging and the National Comprehensive Cancer Network recommend annual screening for women at average risk for breast cancer beginning at age 40 and continuing as long as the woman is in good health.
In the study, Dr. Monticciolo and colleagues performed a secondary analysis of Cancer Intervention and Surveillance Modeling Network (CISNET) 2023 median estimates of breast cancer screening outcomes. CISNET modeling data gives researchers the opportunity to estimate the outcomes of screening at various frequencies and starting ages using U.S. data.
The researchers compared the benefits of screening, including mortality reduction, life years gained, breast cancer deaths averted, and its risks—including benign, or unnecessary, biopsies and recall rates—for four different scenarios: biennial screening of women 50-74 (the longstanding USPSTF recommendation), biennial screening of women 40-74 (the task force’s new draft recommendation), annual screening 40-74, and annual screening 40-79. CISNET does not offer modeling past age 79.
The review of CISNET estimates showed that annual screening of women 40-79 with either digital mammography or tomosynthesis showed a mortality reduction of 41.7%. Biennial screening of women 50-74 and 40-74 showed mortality reduction of 25.4% and 30%, respectively. Annual screening of women 40-79 years showed the lowest per mammogram false-positive screens (6.5%) and benign biopsies (0.88%) compared to other screening scenarios.
“The biggest takeaway point of our study is that annual screening beginning at 40 and continuing to at least age 79 gives the highest mortality reduction, the most cancer deaths averted, and the most years of life gained,” Dr. Monticciolo said. “There’s a huge benefit to screening annually until at least 79 and even more benefit if women are screened past 79.”
Dr. Monticciolo said that although the USPSTF uses CISNET modeling to formulate its recommendations, it refers to recall rates and benign biopsies as harms, rather than risks.
“To balance the harms and benefits of screening mammography, they’re willing to give up some mortality benefit to avoid women being recalled for additional imaging and benign biopsies,” she said.
According to the researchers’ analyses, the chance of a woman having a benign biopsy following annual screening is less than 1%, and all recall rates for screening mammography are under 10%. When screening is performed annually with tomosynthesis, the recall rate decreases to 6.5%.
“The risks of screening are non-lethal and manageable for most women,” she said. “But advanced breast cancer is often lethal. Breast cancer is easier to treat if it’s found earlier; we’re able to spare women extra surgeries and chemotherapy. It’s just a better idea to shift to early detection, and that’s what screening does.”
Dr. Monticciolo said she hopes that her study will add to the body of literature that supports annual screening beginning at age 40 as the best way to diagnose cancer early.
“This paper is important because it shows once again that there’s a tremendous increase in mortality benefit by screening annually between the ages of 40-79, and that the chances of experiencing harm are low on a per-exam basis,” she said. “It comes down to valuing women’s lives. I am hoping that primary care physicians see that risks of screening are manageable, and the benefits are tremendous. We need to do this for women.”
For more information: www.rsna.org
Related Breast Density Content:
VIDEO: Research and Advancements in Breast Imaging Technology
VIDEO: FDA Update on the US National Density Reporting Standard - A Discussion on the Final Rule
One on One … with Wendie Berg, MD, PhD, FACR, FSBI
Creating Patient Equity: A Breast Density Legislative Update
AI Provides Accurate Breast Density Classification
VIDEO: The Impact of Breast Density Technology and Legislation
VIDEO: Personalized Breast Screening and Breast Density
VIDEO: Breast Cancer Awareness - Highlights of the NCoBC 2016 Conference
Fake News: Having Dense Breast Tissue is No Big Deal
The Manic World of Social Media and Breast Cancer: Gratitude and Grief
Related Breast Imaging Content:
Single vs. Multiple Architectural Distortion on Digital Breast Tomosynthesis
Today's Mammography Advancements
Digital Breast Tomosynthesis Spot Compression Clarifies Ambiguous Findings
AI DBT Impact on Mammography Post-breast Therapy
ImageCare Centers Unveils PINK Better Mammo Service Featuring Profound AI
Radiologist Fatigue, Experience Affect Breast Imaging Call Backs
Fewer Breast Cancer Cases Between Screening Rounds with 3-D Mammography
Study Finds Racial Disparities in Access to New Mammography Technology



 February 18, 2026
February 18, 2026 









