May 10, 2019 — Patients with advanced Hodgkin's lymphoma who have large tumors at the time of diagnosis may benefit from radiotherapy after chemotherapy, even when all traces of the cancer appear to have gone. These findings are according to late-breaking results presented at the European Society for Radiotherapy and Oncology (ESTRO) 38 conference, April 26-30 in Milan, Italy.
Approximately 65-70 percent of patients with advanced stage Hodgkin's lymphoma can be cured by receiving six cycles of ABVD chemotherapy — which includes doxorubicin, bleomycin, vinblastine and dacarbazine — with or without subsequent radiotherapy. Currently, however, the addition of radiotherapy is controversial.
In a statement before the conference, Mario Levis, M.D., a co-author of the study, who is a radiation oncologist at the University of Turin, Italy, explained: "These patients can often have four or five decades of life expectancy ahead of them but, given this cure rate, the cancer treatment can result in a high risk of complications for many long-term survivors. For this reason, it's important that we give patients the most effective treatment for curing their cancer, while, at the same time, trying to keep the toxic side effects to a minimum."
To investigate whether radiotherapy after ABVD chemotherapy provided any benefit to these patients, researchers in several centers in Italy, led by Prof. Pier Luigi Zinzani, of the Institute of Haematology at the University of Bologna, and Prof. Umberto Ricardi, head of the Department of Oncology at the University of Turin and president of ESTRO, recruited 512 patients between 2008 and 2013 to a randomized clinical trial, HD0801.
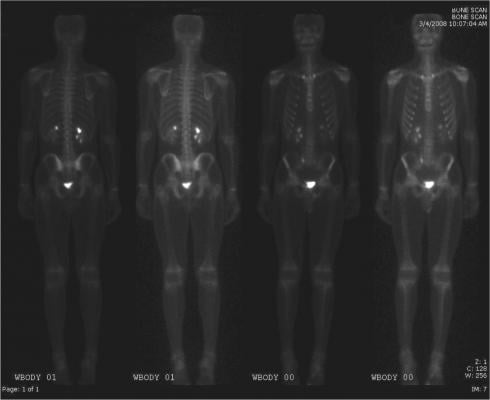
Patients who had been treated successfully in the earlier, phase II part of the trial, and in whom positron emission tomography (PET) scans showed no trace of cancer both during and at the end of chemotherapy, were randomized to the phase III part of the trial to receive either radiotherapy in order to mop up any remaining cancer cells, or no further treatment.
In total, 354 patients had PET scans showing they were clear of cancer after the initial treatment. Of these, 116 (32.7 percent) had had large lesions (greater than 5cm in diameter) at the time of their diagnosis, and they were assigned to radiotherapy or no further treatment.
Levis and Ricardi found that more patients were alive three and five years later without their disease getting worse (known as progression-free survival) if they had been treated with radiotherapy than those who did not receive it.
Ricardi told the conference, "We found that three years later 92 percent of patients who received radiotherapy were still alive without disease progression compared to 82 percent of patients who did not receive it. After five years, these figures were 89 percent and 82 percent respectively. This suggests that patients with large tumors, who have responded to six cycles of ABVD chemotherapy, may still benefit from the addition of radiotherapy, with a survival benefit ranging from 7 to 10 percent at three and five years.
"This is something that should be considered carefully when deciding whether or not to give radiotherapy to these patients. The omission of radiotherapy would guarantee the prevention of radiation-induced toxic side effects, but, on the other hand, it exposes 10 percent of our, frequently young, patients to an increased risk of relapse and of even higher toxicity due to the heavy salvage therapies required when the disease returns," concluded Ricardi.
Nine patients who had been enrolled in the radiotherapy arm of the trial did not actually receive radiation treatment due to decisions made by their doctors, and the disease returned in five of them. This meant that when the data on the 116 patients were analyzed according to "intention to treat" (i.e. regardless of whether or not they had actually received the radiotherapy), there was little difference between the two groups in progression-free survival at three and five years. It was only when the researchers analyzed the data according to the treatments the patients had actually received (a "per protocol" analysis) that it was possible to see the benefit on survival for those treated with radiotherapy, although this was not statistically significant. This was mainly because of the small number of patients in whom the disease returned: five in the radiotherapy arm and 13 in the 'no further treatment' arm of the trial.
"The results of this trial do not provide definitive evidence on the role of radiotherapy after chemotherapy for patients with advanced Hodgkin's lymphoma and large tumors. However, the improvement in survival among those who did receive radiotherapy is not negligible. We think that the next step is for a meta-analysis of this and similar randomized trials in order to increase the robustness of the information we have on the best way to treat this disease," concluded Ricardi.
Prof. Yolande Lievens, past-president of ESTRO and head of the department of radiation oncology at Ghent University Hospital, Belgium, said, "As physicians our main aim is to treat our patients effectively while keeping any adverse side-effects from the treatment to the minimum. This is especially important for patients with a disease such as Hodgkin's lymphoma, many of whom can expect to be cured and live long after their treatment has finished. The results from this trial provide us with additional, important information to take into account when advising our patients on what might be the best treatment."
For more information: www.estro.org


 February 04, 2026
February 04, 2026 









