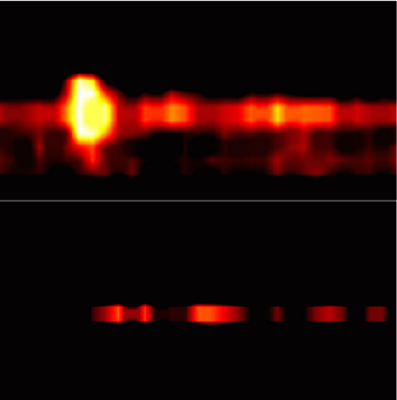
Images of prostate cells captured through photoacoustic imaging. Top: cancer cells that express the targeted cancer marker, PSMA; bottom: cells that lack PSMA. A research team led by Kent Nastiuk of Roswell Park Cancer Institute has published new evidence that this approach can be a useful tool in monitoring and selecting treatments for many cancers.
While active surveillance is often recommended for patients with nonaggressive prostate cancer to reduce unnecessary treatment, the challenge for clinicians is to monitor and distinguish early-stage tumors from advanced cancers. A team of scientists led by researchers from Roswell Park Cancer Institute have demonstrated that photoacoustic imaging (PAI) may be an effective tool for more accurately viewing and monitoring prostate cancer. The new research has been published in the June 2016 issue of the Journal of Biomedical Optics.
Photoacoustic imaging is an emerging noninvasive imaging modality that has not yet been used in clinical settings. Using photoacoustic imaging, this team of scientists focused a laser light on prostate cells and then “listened” using ultrasound technology to see how a dye attached to a specific prostate cancer marker, PSMA, reacted to the light waves. They chose to study this technology’s use in imaging prostate cancer, as the prostate can be imaged in situ. Photoacoustic imaging of these prostate cells, the researchers found, enabled good discrimination between cells with and without the cancer marker.
“This proof-of-concept study demonstrates that this technology may allow for real-time monitoring of prostate cancer in patients during the course of active surveillance. For patients with more aggressive disease, the technology could offer more precise targeting of biopsies to confirm the need for definitive therapy,” said senior author of the study Kent Nastiuk, Ph.D., assistant professor of cancer genetics and genitourinary cancers at Roswell Park. “This technology offers the potential to confirm the initial prostate cancer diagnosis, guide biopsies and monitor tumor volume — which is currently not measureable — for improved case management and treatment decision-making.”
Nastiuk’s co-authors include scientists from Roswell Park Cancer Institute, the University of Rochester and the Rochester Institute of Technology.
The study, “Photoacoustic Imaging with an Acoustic Lens Detects Prostate Cancer Cells Labeled with PSMA-targeting Near Infra-red Dye-conjugates,” is available at biomedicaloptics.spiedigitallibrary.org.
This work was supported by the National Cancer Institute (project nos. R01CA151753, R15CA192148 and P30CA16056), National Institute of Biomedical Imaging and Bioengineering (project no. R15EB019726), National Institute of Arthritis and Musculoskeletal and Skin Diseases (project no. P30AR061307), the U.S. Department of Defense (award no. W81XWH-14-1-0242) and the Sonya A. Sinicki Foundation for Cancer Research (award 615SF).


 February 05, 2026
February 05, 2026