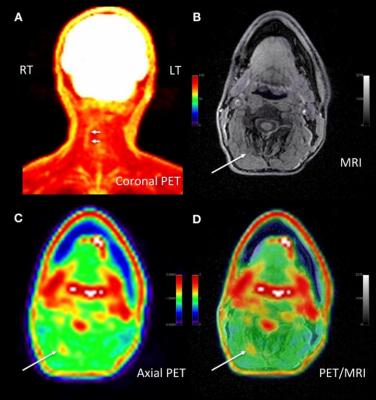
Adult male with decades of right neck pain, discomfort and tightening following birth injury. The patient had failed multiple standard therapeutic maneuvers before presenting for 18F-FDG PET/MR imaging. Images shows abnormally elevated FDG uptake (white arrows; SUVmax = 1.2) observed in a linear pattern in the space in the posterolateral right neck, between the oblique capitis inferior and the semispinalis capitis muscles, where the greater occipital nerve resides. By comparison, the same region on the contralateral, asymptomatic side of the neck has an SUVmax = 0.7. This result encouraged a surgeon to explore the area. The surgeon ultimately found a collection of small arteries wrapped around the nerve in this location. The small arteries underwent lysis by the surgeon and the patient reported tremendous relief of symptoms. (A) Coronal thick slab MIP of 18F-FDG PET. (B) Axial LAVA FLEX MRI through the cervical spine. (C) Axial PET at the same slice as the axial MRI. (D) Fused axial PET/MRI. Image courtesy of Cipriano, et al., Stanford University, CA.
July 14, 2020 — A new molecular imaging approach utilizing 18F-FDG positron emission tomography (PET) and magnetic resonance imaging (MRI) can precisely identify the location of pain generators in chronic pain sufferers, often precipitating a new management plan for patients. This research was presented at the Society of Nuclear Medicine and Molecular Imaging 2020 Annual Meeting.
Pain is the most common reason to seek medical attention, and those who suffer from it outnumber those who suffer from cancer, heart disease and diabetes combined. According to the National Center for Complementary and Integrative Health, chronic pain affects nearly 50 million adults in the United States and costs the nation's healthcare system as much as $635 billion in total expenses, including imaging and treatment costs.
"In the past few decades, we have confirmed that anatomic-based imaging approaches, such as conventional MRI, are unhelpful in identifying chronic pain generators," said Sandip Biswal, M.D., musculoskeletal radiologist and associate professor of radiology at Stanford University School of Medicine in Stanford, California. "We know that 18F-FDG PET has the ability to accurately evaluate increased glucose metabolism that arises from to acute or chronic pain generators. As such, in our study we examined PET/MRI as a potential solution to determine the exact molecular underpinnings of one's pain."
In the study, 65 chronic pain patients underwent 18F-FDG PET/MRI from head to foot. Maximum standardized uptake values and target-to-background ratios were measured using image analysis software. PET/MR images were evaluated by two radiologists to determine if increased 18F-FDG uptake occurred in the site of symptoms or in other areas of the body. Imaging results were then discussed with the referring physician, who determined whether a change in the pain management plan would follow.
Increased uptake of 18F-FDG in affected nerves and muscle was identified at the site of pain and other areas of the body in 58 out of 65 patients. This resulted in a mild modification of management plan (e.g., additional diagnostic test) for 16 patients and a significant modification for 36 patients (e.g., new invasive procedure suggested or ordered). In total, new management plans were implemented for 40 out of 65 patients, which had not been anticipated by the referring physician.
"The results of this study show that better outcomes are possible for those suffering from chronic pain," said Biswal. "This clinical molecular imaging approach is addressing a tremendous unmet clinical need, and I am hopeful that this work will lay the groundwork for the birth of a new subspecialty in nuclear medicine and radiology. Using this approach will require knowledge and expertise not only in nuclear medicine but also in musculoskeletal imaging, neuroradiology and potentially other fields, such as body imaging and pediatric radiology, where pain syndromes are important clinical problems."
For more information: www.snmmi.org
Related SNMMI20 Content:
PSMA PET/CT Can Change Management in Recurrent Prostate Cancer
Total-body Dynamic PET Successfully Detects Metastatic Cancer
New PET Radiotracer Proven Safe in Imaging Malignant Brain Tumors
Targeted Radionuclide Therapy Enhances Prostate Cancer Response to Immunotherapies
New PET/MRI Approach Pinpoints Chronic Pain Location, Alters Management


 February 03, 2026
February 03, 2026