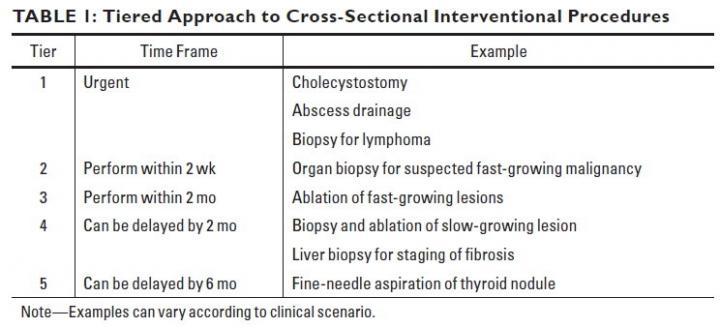
For procedural delays that will not adversely affect patient outcome, Fananapazir and colleagues proposed the following tiered approach for both outpatient and inpatient scenarios: urgent procedures, procedures that should be performed within 2 weeks, procedures that should be performed within 2 months, and procedures that can safely be delayed 2 or 6 months. Courtesy of American Journal of Roentgenology (AJR)
June 5, 2020 — An open-access article in the American Journal of Roentgenology (AJR) details myriad practical updates that radiologists performing cross-sectional interventional procedures should institute to minimize risks for patients and imaging personnel alike during the coronavirus disease (COVID-19) pandemic.
"Cross-sectional interventional procedures are performed under CT, ultrasound, fluoroscopy, or MRI guidance and include fluid aspiration, (thoracentesis, paracentesis, and fluid collections), drainage catheter placement, percutaneous biopsy, and tumor ablation," explained lead author Ghaneh Fananapazir at the University of California Davis Medical Center.
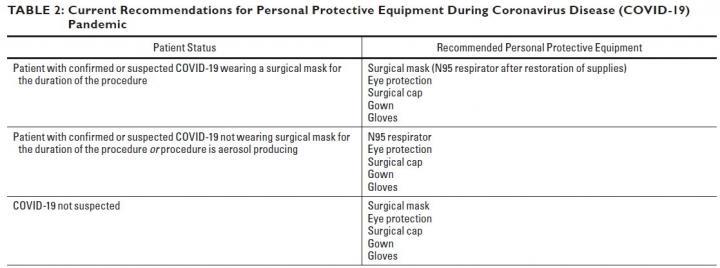
All of these procedures require appropriate donning and doffing of personal protective equipment by every member of the IR team — physician, trainee, nurse, technologist — and some procedures may require admitting the patient for management of postprocedure complications, necessitating a hospital bed and auxiliary resources.
Thus, for procedural delays that will not adversely affect patient outcome, Fananapazir and colleagues proposed the following tiered approach for both outpatient and inpatient scenarios: urgent procedures, procedures that should be performed within 2 weeks, procedures that should be performed within 2 months, and procedures that can safely be delayed 2 or 6 months.
"Each procedure request must be triaged into a tier on a case-by-case basis," Fananapazir et al. warned, "because clinical circumstances can dictate one procedure as urgent, whereas different clinical data may render the same procedure safe to delay." When considering any procedural delay, Fananapazir's team strongly recommended consultation with the referring physician, who may have insights not available to the interventional radiologist.
Wherever possible, procedures should be performed bedside in COVID-19 units (or patient rooms, should no dedicated COVID-19 unit exist). Regarding ultrasound-guided procedures, specifically, a mobile ultrasound unit can be left in place in the ICU or the COVID-19 unit — "used for interventional procedures, guidance for vascular access, or point-of-care thoracic and nonthoracic ultrasound," wrote Fananapazir et al. Ultrasound probes should be sterilized according to manufacturer guidelines.
Fananapazir's team also cautioned against computed tomography (CT) technologists or sonographers entering the procedure room. Ideally, all anticipated IT tray supplies should be acquired before the procedure commences, covered with a sterile plastic drape, and opened only to the extent needed.
Additionally, patient interaction during the informed consent interview can be limited by obtaining consent in the procedure room or using documented oral consent in the medical record. "Both of these modifications to the consent process are outside of standard regulated practice," the authors of this AJR article noted, "therefore, establishment of hospital-wide frameworks may be needed."
For more information: www.
Related Coronavirus Content:
VIDEO: Imaging COVID-19 With Point-of-Care Ultrasound (POCUS)
The Cardiac Implications of Novel Coronavirus
CT Provides Best Diagnosis for Novel Coronavirus (COVID-19)
Radiology Lessons for Coronavirus From the SARS and MERS Epidemics
Deployment of Health IT in China’s Fight Against the COVID-19 Epidemic
Emerging Technologies Proving Value in Chinese Coronavirus Fight
Radiologists Describe Coronavirus CT Imaging Features
Coronavirus Update from the FDA
CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia
CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV)
Chest CT Findings of Patients Infected With Novel Coronavirus 2019-nCoV Pneumonia
Find more related clinical content Coronavirus (COVID-19)
ACC COVID-19 recommendations for the cardiovascular care team
VIDEO: What Cardiologists Need to Know about COVID-19 — Interview with Thomas Maddox, M.D.
The Cardiac Implications of Novel Coronavirus
ESC Council on Hypertension Says ACE-I and ARBs Do Not Increase COVID-19 Mortality


 February 09, 2026
February 09, 2026 









