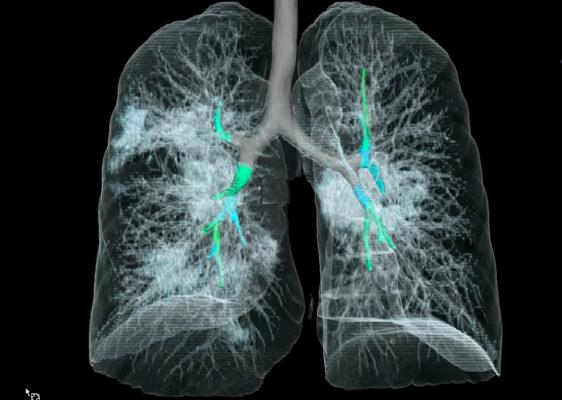
CT lung imaging from a 41-year-old woman who tested positive for the 2019 novel coronavirus (2019-nCoV). This 3-D reconstruction shows multifocal ground glass opacities without consolidation. See also three-dimensional VIDEO of this rendering.
February 5, 2020 — In a special report published in the journal Radiology, researchers describe computed tomography (CT) imaging features that aid in the early detection and diagnosis of Wuhan coronavirus.
“Early disease recognition is important not only for prompt implementation of treatment, but also for patient isolation and effective public health surveillance, containment and response,” said the study’s lead author, Michael Chung, M.D., assistant professor in the Department of Diagnostic, Interventional and Molecular Radiology in the Mount Sinai Health System in New York, N.Y.
On Dec. 31, 2019, the World Health Organization (WHO) learned of several cases of a respiratory illness clinically resembling viral pneumonia and manifesting as fever, cough and shortness of breath. The newly discovered virus emerging from Wuhan City, Hubei Province of China, has been temporarily named “novel coronavirus” (2019-nCoV). This new coronavirus belongs to a family of viruses that include Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS).
The outbreak is escalating quickly, with thousands of confirmed 2019-nCoV cases reported globally. On Jan. 30, the U.S. reported the first confirmed instance of person-to-person spread of the virus.
 In this retrospective case series, Chung and colleagues set out to characterize the key chest CT imaging findings in a group of patients infected with 2019-nCoV in China with the goal of familiarizing radiologists and clinical teams with the imaging manifestations of this new outbreak.
In this retrospective case series, Chung and colleagues set out to characterize the key chest CT imaging findings in a group of patients infected with 2019-nCoV in China with the goal of familiarizing radiologists and clinical teams with the imaging manifestations of this new outbreak.
From Jan. 18, 2020, until Jan. 27, 2020, 21 patients admitted to three hospitals in three provinces in China with confirmed 2019-nCoV infection underwent chest CT. The 21 patients consisted of 13 men and 8 women ranging in age from 29 to 77 years old, with a mean age of 51.2 years. All patients were confirmed positive for infection via laboratory testing of respiratory secretions.
For each of the 21 patients, the initial CT scan was evaluated for the following characteristics:
• (1) presence of ground-glass opacities;
• (2) presence of consolidation;
• (3) number of lobes affected by ground-glass or consolidative opacities;
• (4) degree of lobe involvement in addition to overall lung “total severity score;”
• (5) presence of nodules;
• (6) presence of a pleural effusion;
• (7) presence of thoracic lymphadenopathy (lymph nodes of abnormal size or morphology); and
• (8) presence of underlying lung disease such as emphysema or fibrosis. Any other thoracic abnormalities were also noted.
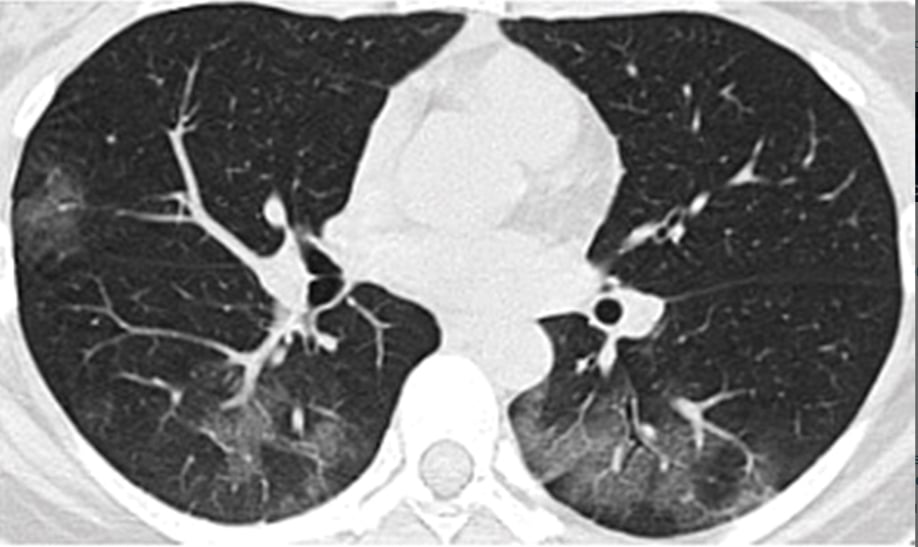
Radiological Presentation of Coronavirus on CT Imaging
The analysis showed that 2019-nCoV typically manifests on CT with bilateral ground-glass and consolidative pulmonary opacities. Nodular opacities, crazy-paving pattern, and a peripheral distribution of disease may be additional features helpful in early diagnosis. The researchers also noted that lung cavitation, discrete pulmonary nodules, pleural effusions and lymphadenopathy are characteristically absent in cases of 2019-nCoV.
Follow-up coronavirus imaging in seven of eight patients showed mild or moderate progression of disease as manifested by increasing extent and density of airspace opacities.
Chung cautioned that absence of abnormal CT findings upon initial examination does not rule out the presence of 2019-nCoV.
“Our patient population is unique from other published series on the Wuhan coronavirus in that three of our patients had normal initial chest CTs,” he said. “One of these patients progressed three days later and developed a solitary nodular ground-glass lesion in the right lower lobe, indicating this pattern may represent the very first radiologically visible manifestation of disease in some patients infected with Wuhan coronavirus.”
He added that a second patient had a normal follow-up chest CT four days after her initial normal imaging exam.
“This suggests that chest CT lacks complete sensitivity and does not have a perfect negative predictive value,” Chung said. “We can’t rely on CT alone to fully exclude presence of the virus.”
“We can’t rely on CT alone to fully exclude presence of the virus.”
This finding may be related to the fact that infection with 2019-nCoV is characterized by an incubation period of several days, and there may be a phase where viral infection manifests with symptoms prior to visible abnormalities on computed tomography.
The researchers note that further study is required to understand how patients fare after treatment but suggest that experience and imaging findings from MERS and SARS epidemics might be helpful in managing the current outbreak.
Chung’s colleagues at Mount Sinai include cardiothoracic radiologist Adam Bernheim, M.D., and Ph.D. candidate Xueyan Mei. Colleagues in China, including Hong Shan, M.D., from Guangdong Provincial Key Laboratory of Biomedical Imaging, The Fifth Affiliated Hospital of Sun Yat-sen University in Zhuhai (Guangdong Province) were also instrumental in this work.
The special report is accompanied by “Chest CT Findings in 2019 Novel Coronavirus (2019-nCoV) Infections from Wuhan, China: Key Points for the Radiologist,” by Jeffrey P. Kanne, M.D., from the University of Wisconsin School of Medicine and Public Health.
How Clinicians Can Keep Track of the Coronavirus Spread
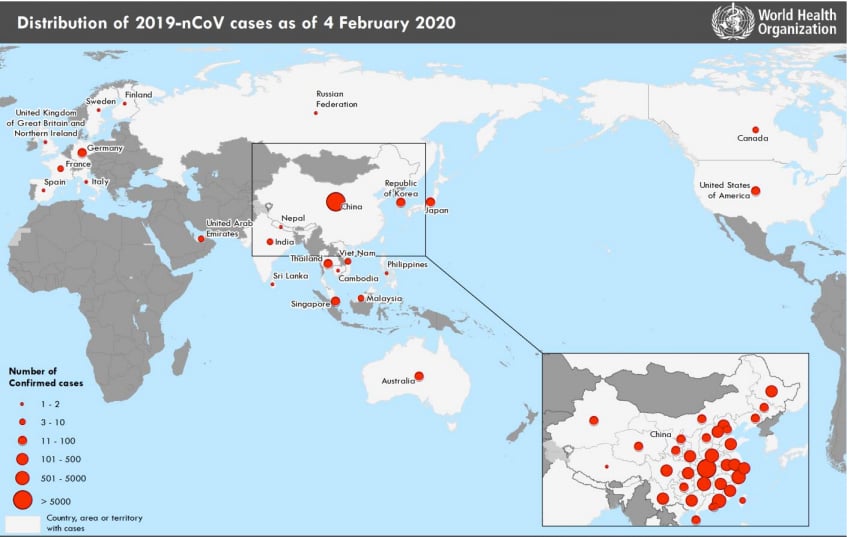
Corona virus (2019 nCoV) situation map as of Feb. 5, 2020 from the World Health Organization (WHO).
As of Wednesday, Feb. 5, 2020, the World Health Organization (WHO) listed the following statistics on the spread of thee coronavirus:
• 20,630 confirmed 2019-nCoV cases globally
• 20,471 of these cases are in China
• 159 cases are confirmed outside of China in 23 countries
• 425 deaths reported, all but 1 are in China
The U.S. Food and Drug Administration (FDA) took steps in the coronavirus response effort Feb. 4, issuing an emergency use authorization for the first 2019 novel coronavirus diagnostic test. The Centers for Disease Control and Prevention (CDC) was using this test to confirm patients infected with the nCoV2019 virus and it is now released for use by qualified clinical labs.
The CDC coronavirus page is located at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
ECRI Institute has developed a Coronavirus Outbreak Preparedness Center to help hospitals protect healthcare workers and patients as the threat of coronavirus rapidly spreads across the globe. ECRI’s Coronavirus Outbreak Preparedness Center includes:
• Preparation and patient handling checklists
• Equipment and alternative suppliers
• Patient care equipment evaluations, including portable ventilators
• Recommendations for infection control
• Resources from Centers for Disease Control and World Health Organization
Related Coronavirus Imaging Content:
CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia
Infervision in the Frontlines Against the Coronavirus
CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV)
The Cardiac Implications of Coronavirus
Find more related clinical content Coronavirus (COVID-19)


 February 09, 2026
February 09, 2026 









