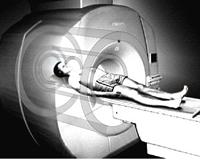
July 18, 2011 – Driving new technologies that will help expand the availability of MRI scanners beyond the hospital to smaller clinic settings, GE Global Research, the technology development arm for the General Electric Company, and the Mayo Clinic have received a five-year, $5.7 million grant from the National Institute of Biomedical Imaging and Bioengineering (NIBIB) and the National Institute of Neurological Disorders and Stroke (NINDS), components of the National Institutes of Health (NIH). They will jointly conduct research to understand design and application issues involved in the use of a dedicated magnetic resonance imaging (MRI) brain scanner to image for a range of neurological and psychiatric disorders such as stroke, Alzheimer’s Disease, Parkinson’s Disease, traumatic brain disorder (TBI), depression and autism.
The team at the Mayo Clinic collaborating with GE is led by Matt A. Bernstein, Ph.D., a medical physicist, and John Huston III, M.D., a neuroradiologist. Together they will explore how this innovative technology can be utilized to improve medical diagnosis while also reducing costs.
“The development of a head-only MRI system can address 25-30 percent of all MR imaging procedures today,” said Jim Davis, general manager of GE Healthcare’s MRI business. “Research in this area brings benefits of lower total costs, better image quality, greater patient comfort and makes this a very attractive opportunity for collaboration.”
Steve Williams, professor of imaging sciences and founder of the Department of Neuroimaging at the Institute of Psychiatry at King’s College London, believes the development of a dedicated MRI brain scanner has tremendous potential in the field of psychiatry. “A smaller, lighter, dedicated head-only MRI system will have a huge positive impact on the field of psychiatry. During the past decade, brain imaging research has dramatically improved our understanding of mental illness. The creation of dedicated head-only MRI system will take our clinical implementation to the next level.”
Williams added, “A head-only MR system will make neurological and psychiatric examinations of all age groups so much easier. Patient access and management will be enhanced without compromising image quality or scanner performance.”
The intention is that a dedicated high-field scanner could offer a more specialized imaging approach and a greater range of functionality for neurological imaging compared to the current one-size-fits-all concept of whole-body MRI imaging. The goal of the program is ultimately to understand and address the technical issues involved in dedicated MR imaging of the brain.
“Today, MRI scanners are most often associated with big hospital or clinic settings, which limit patient access to this important technology,” said Thomas K. Foo, manager, chief scientist, Diagnostic and Biomedical Technologies at GE Global Research. “Research on this dedicated brain MRI scanner prototype could potentially help expansion of MRI into smaller community hospitals and rural settings, reaching millions more patients globally. We want to bring neurological imaging and care closer to where patients can access it, no matter where they live.”
“We are excited about this public-private partnership to develop specialized MRI scanners that are lower in costs and more accessible to a broader community,” said Belinda Seto, deputy director, NIBIB.
“Brain science and the care of patients with brain disorders has markedly advanced with the advent of modern MRI technology,” said Walter J. Koroshetz, M.D., deputy director of the NINDS. “Research leading to the development of a compact brain MRI system would offset the high power and cooling requirement of the large machines currently in use and would bring this valuable technology to all areas of the United States, military in service to their country and people around the world.”
This NIH-funded collaboration between GE and Mayo Clinic illustrates an emerging trend of more specialized imaging systems. With a dedicated approach, MRI scanners can be more specifically tailored and designed for neurological imaging applications that lead to improved image quality and a more comfortable experience for the patient. It also will enable smaller, lighter designs that increase the accessibility of MRI to remote settings and regions where the technology is currently unavailable. The project is closely aligned with GE’s “Healthymagination” initiative, which is built on a global commitment to reduce costs, improve quality and expand access to healthcare for millions of people.
Compared to equivalent field strength whole-body MRI scanner, GE’s prototype scanner is expected to deliver the same (or better) quality images, but from a scanner that is only one-third the size and significantly lighter.
Beyond removing major siting barriers, GE researchers will be incorporating new image analysis tools and easier-to-use operating systems and interfaces that expand the system’s imaging capabilities and enable more healthcare professionals to acquire diagnostic images. For example, new “one-touch” features are being developed that will simplify the programming of image settings from dozens of complex inputs to a single control.
“With a dedicated approach, we can develop an imaging platform that is more robust and easier to use to help medical providers assess and diagnose a broader range of neurological and psychiatric disorders,” Foo said. “We can go one level deeper in functionality than we could with a standard MRI whole-body system.”
GE researchers will develop and complete the prototype system over the next three years. It will then be tested in human clinical trials at Mayo Clinic in Rochester, Minn., for the remaining two years of the project. During that time, the system will be assessed and compared to standard MRI scanners used today.
For more information: www.ge.com/research, www.MayoClinic.com


 January 28, 2026
January 28, 2026 









