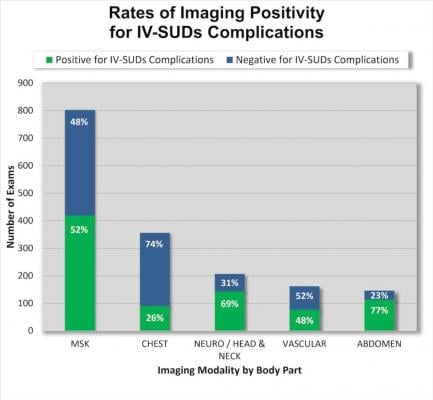
Rates of Imaging Positivity for IV-SUDs Complications. Image courtesy of Efren J. Flores, M.D.
January 11, 2018 – Emergency radiologists are seeing a high prevalence of patients with complications related to opioid use disorders, according to results from a 12-year study presented at the annual meeting of the Radiological Society of North America (RSNA), Nov. 26-Dec. 1 in Chicago. Researchers said the findings underscore the need for radiologists to play a role in the care continuum for these patients.
Substance use disorders of highly addictive opioids like heroin, fentanyl and oxycodone continue to skyrocket in the U.S. Intravenous opioid use disorders are a major contributor to the drug overdoses that are the leading cause of injury and death in the United States, according to the Department of Health and Human Services. Patients prescribed opioid medications for pain management of a medical condition often develop dependence, and many go from crushing and injecting pills to injecting heroin as a less expensive way to deal with their disease, said senior study author Efren J. Flores, M.D., emergency radiologist at Massachusetts General Hospital in Boston.
“We’ve seen a dramatic increase in the past year of patients coming into the emergency department with complications related to substance use disorders,” he said. “The patient population is underserved. By the time we see them, they have more advanced complications because they’re hesitant to ask for help due to social stigmas.”
For the study, Flores and colleagues looked at the prevalence and type of complications related to substance use disorders in patients arriving at emergency radiology. The study group included 1,031 patients imaged from 2005 to 2016 for substance use-related complications. Of all the patients, 66 percent were men, 78 percent were white and the mean age was 36 years.
The results showed a high prevalence of complications among the patients, including symptoms related to injections, respiratory issues and back pain.
“Complications were most frequently related to skin and soft tissue infections caused by the use of non-sterile needles,” Flores said. “In some cases, we found septic emboli in the lung or brain. As these patients start having to access larger veins, they become more prone to these types of infections.”
There were 1,673 imaging exams performed, including 779 X-rays, 544 computed tomography scans (CTs), 292 magnetic resonance imaging scans (MRIs) and 58 ultrasounds. Imaging results often provided critical information, such as when physicians changed the management plan for a patient with a substance-abuse-related lumbar spine infection after CT scans showed the involved nerves.
History of opioid prescriptions before the first imaging exam was present in 310 (30 percent) cases with a mean of 10 prescriptions per patient. History of opioid prescriptions was significantly higher in women (36 percent, 128/352), than men (27 percent, 182/679). Mean time from opioid prescription to first imaging exam was 51 months – significantly shorter in men (45 months) than women (51 months).
Overall, 121 of the 1,031 patients, or 11.7 percent, died before the end of the study period. The mortality rate was 14 percent for patients with a positive imaging diagnosis of substance-abuse-related complications – significantly higher than the 10 percent rate for patients with no such history. Five-year mortality rates were also higher in patients with prior opioid prescriptions and with imaging complications.
The prevalence of substance use disorder in patients presenting to emergency radiology provides radiologists a unique opportunity to “look beyond the reading room, and see other ways we can help,” Flores said. For instance, radiologists can encourage patients to use sterile needles, inform them about needle exchange programs and advise them to use alcohol at the injection site to avoid infections. Radiologists can also help steer patients into programs or connect them with recovery coaches, both in the hospital and community, to help them with their illness.
“Radiology is central to patient care in the emergency department setting,” Flores said. “We need to be actively advocating for these patients and giving them an opportunity to take steps into recovery.”
Co-authors are Renata R. Almeida, M.D., Mohammad Mansouri, M.D., M.P.H., Ajay K. Singh, M.D., and Michael H. Lev, M.D.
For more information: www.rsna.org
Related Content


 February 13, 2026
February 13, 2026 









