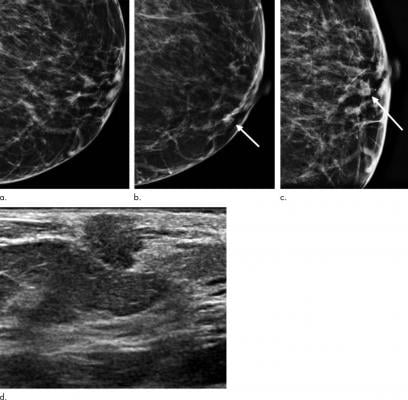
Images show symptomatic false-negative cancer in a 73-year-old black woman who presented with a palpable abnormality 64 days after negative screening mammography. (a) Negative screening left digital breast tomosynthesis (DBT) mammogram. (b) Diagnostic DBT mammogram shows a new palpable mass (arrow). (c) Spot-compression DBT mammogram enables confirmation of mass (arrow). (d) Ultrasound (US) image shows hypoechoic mass with angular margins. Subsequent US-guided biopsy revealed estrogen receptor- and progesterone receptor-positive and human epidermal growth factor receptor 2-negative invasive ductal carcinoma. Image courtesy of Radiological Society of North America
December 7, 2020 — Breast cancer screening with digital breast tomosynthesis (DBT) offers significant advantages over digital mammography, including improved cancer detection and lower false negative rates, according to a study published in Radiology.
In DBT, an X-ray camera moves in an arc over the breast, acquiring images from different angles. The pictures are processed into a 3D-like image that can be scrolled through a millimeter at a time. This eliminates the problem of overlapping tissue that often hides cancers and results in recalls for additional imaging in digital mammography.
"With DBT, you can really feel like you're combing through the breast tissue instead of just looking at flat pictures," said study lead author Melissa A. Durand, M.D., associate professor of diagnostic radiology and biomedical imaging at Yale University School of Medicine and Smilow Cancer Hospital in New Haven, Connecticut.
While research has illuminated DBT's edge over digital mammography in cancer detection, its impact on patient survival has not been established.
For the new study, Durand and colleagues looked at more than 380,000 screening examinations to compare the performance of DBT and digital mammography. Among the performance metrics they assessed were the rates of false negative screening examinations, or cancers detected within a year of a normal mammogram. Since false negative cancers tend to be more aggressive than screen-detected cancers, a reduction in them may be considered a surrogate for longer-term screening outcomes such as advanced disease or death.
"Using false negative cancer rates is a way to get an idea of how a tool can affect morbidity/mortality in a more reasonable time frame than a randomized clinical trial," Durand said.
Analysis showed that screening with DBT improved sensitivity and specificity for breast cancer and identified more invasive cancers with fewer nodal or distant metastases.
"Our results build on past studies that have shown that DBT improves performance outcomes for breast cancer screening," Durand said. "With DBT, we show we are detecting more invasive cancers, but they are cancers with favorable prognostic criteria, which means these patients would have more treatment options."
Screening with DBT demonstrated a trend toward lower rates for overall false negatives and symptomatic false negatives, or those that present with a symptom like pain, discharge or a lump.
The results also showed advantages for DBT in imaging women with mammographically dense breasts, or breasts with a higher proportion of fibrous and glandular tissue compared with fatty tissue. Cancers can be more difficult to see in dense breasts, and breast density itself is a risk factor for cancer.
Recall rates were significantly lower in both heterogeneously dense breasts — those with mostly dense tissue but with some areas of non-dense tissue--and extremely dense breasts in the DBT group compared to digital mammography.
"We also saw significantly higher cancer detection rates with DBT in women with heterogeneously dense breasts compared to digital mammography," Durand said. "With women who have extremely dense breasts, the cancer detection was higher, but not significantly so, which makes sense. You need a bit of fat to provide contrast to the fibroglandular tissue in order to detect abnormalities, whether you are using DBT or digital mammography. This highlights a group of women who would benefit from supplementary screening."
The study results add to a growing body of literature supporting DBT for regular breast cancer screening. Its superior cancer detection translates to fewer recalls and fewer additional imaging exams needed.
While DBT studies carry a higher radiation dose than that of 2D mammography, a technique known as synthesized DBT essentially halves the radiation dose.
"Together with reduced recall rates and, thus, less patient anxiety, I would anticipate that DBT will continue to move forward as the standard of care to replace regular mammography," Durand said.
For more information: www.rsna.org


 February 17, 2026
February 17, 2026 









