RELATED CONTENT
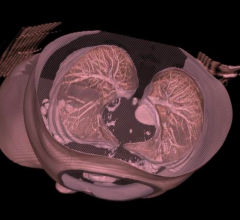
The American College of Radiology said it is deeply disappointed at the failure of the Medicare Evidence Development & Coverage Advisory Committee (MEDCAC) to vote in support of national Medicare coverage of low-dose computed tomography (LDCT) screening for patients at high risk for lung cancer.
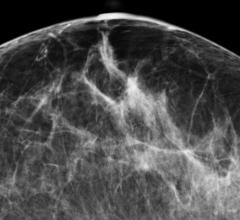
Anxiety regarding inconclusive test results is real and is only natural. Experts in breast imaging (researchers and clinicians) continue to work to reduce the number of false-positive exams that patients experience and ensure that follow-up exams are as minimally invasive as possible.
Congress recently passed the Protecting Access to Medicare Act of 2014 (H.R. 4302) that delays a 24 percent Medicare physician payment cut for 12 months. The legislation also requires use of appropriate use criteria (AUC) and clinical decision support (CDS) software to get Medicare reimbursement, which will likely shift focus onto IT vendors who can supply this software. In addition, the use of CDS is part of Stage 2 Meaningful Use requirements for electronic medical records (EMR), so the new Medicare requirements will move CDS up on many IT departments’ priority lists.
April 24, 2014 — At an April 30 meeting, Ella Kazerooni, M.D., chair of the American College of Radiology (ACR) Committee on Lung Cancer Screening, will urge the 2014 Medicare Evidence Development and Coverage Advisory Committee (MedCAC), to recommend national Medicare coverage of low-dose computed tomography (LDCT) screening for patients at high risk for lung cancer.
The American College of Radiology (ACR) strongly supports several provisions in the bipartisan “Protecting Access to Medicare Act of 2014,” introduced in the House of Representatives to ward off drastic Medicare provider reimbursement cuts mandated by the flawed sustainable growth rate (SGR) physician payment formula.
The American College of Radiology applauded steps to reign in medical imaging and radiation oncology self-referral included in President Obama’s Fiscal Year 2015 budget. However, prior authorization for imaging services, also included the FY 2015 budget, is unnecessary and will ultimately raise costs, interfere in the doctor-patient relationship and restrict ready access to imaging care.
The American College of Radiology (ACR) strongly supports the bicameral, bipartisan legislation to replace the sustainable growth rate (SGR) payment formula. The organization particularly applauds inclusion of several ACR backed provisions that raise quality of care, make care more efficient and increase transparency in physician payment policy.
Breast imagers worldwide now have access to the fifth edition of the American College of Radiology (ACR) Breast Imaging Reporting and Data System (BI-RADS) Atlas. This edition is designed to improve patient care by serving as a comprehensive guide providing standardized breast imaging terminology, report organization, assessment structure and a classification system for mammography, ultrasound and magnetic resonance imaging (MRI) of the breast.
According to the American College of Radiology and Society of Breast Imaging, the recent article (O’Donoghue et al) regarding costs of national breast cancer screening published in the Annals of Internal Medicine (AIM) is misleading and provides an incomplete picture of costs and benefits of breast cancer screening programs.


 May 07, 2014
May 07, 2014