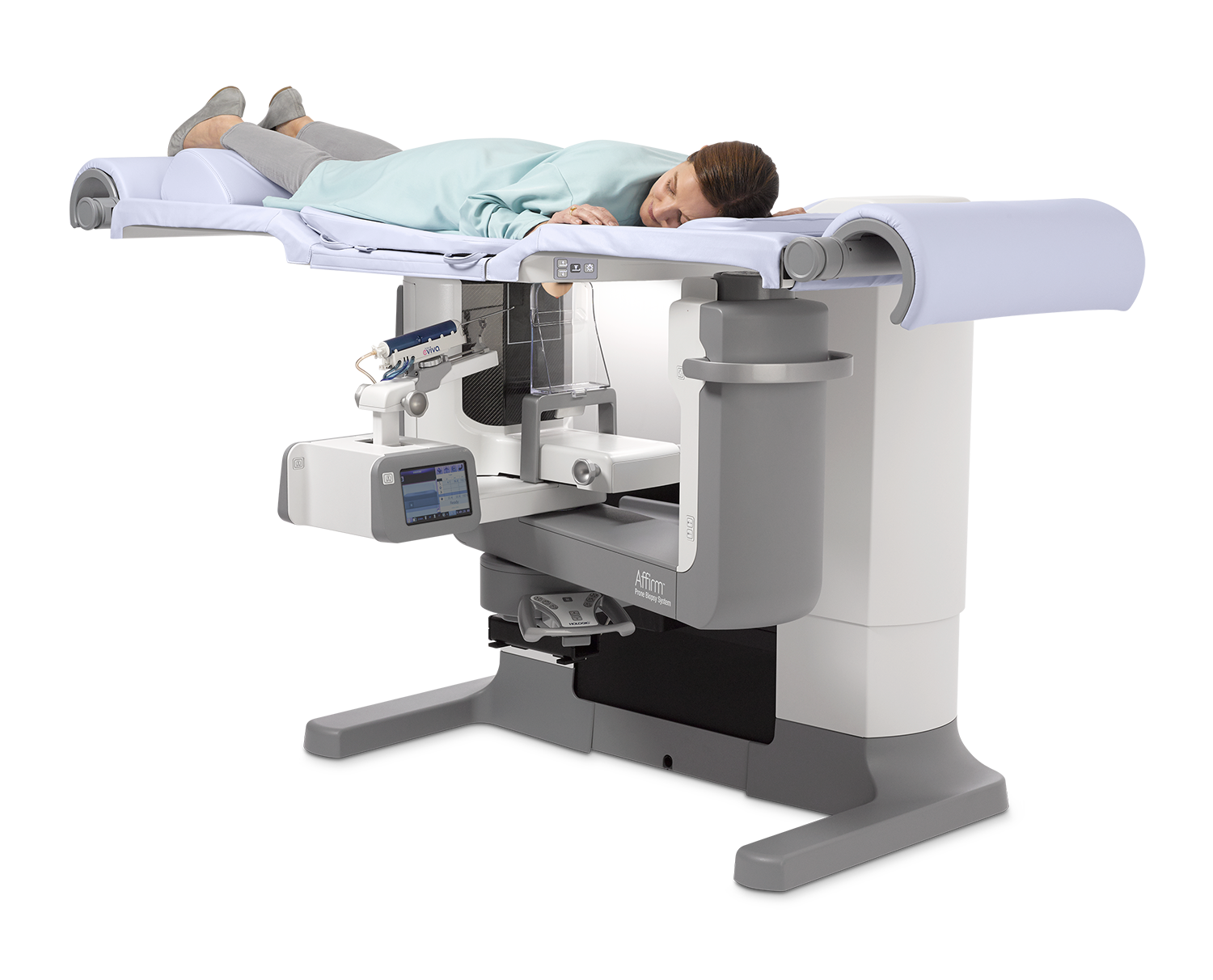
A patient prepares to have a tomosynthesis-guided prone breast biopsy using the Hologic Affirm prone biopsy system.
The current body of research supporting digital breast tomosynthesis (DBT or 3-D mammography) is now overwhelming, with numerous single and multi-institutional studies showing this technology improves screening outcomes and accuracy by increasing breast cancer detection rates, decreasing recall rates and increasing specificity. Since DBT debuted in 2011, its utilization has quickly increased.
A recent JAMA Internal Medicine1 research letter showed that use of DBT for breast cancer screening has grown rapidly, increasing from almost 13 percent of screening exams in 2015 to more than 43 percent in 2017. More than 93 percent of insured women now have coverage for DBT exams. The American Society of Breast Surgeons’ (ASBrS) newly released, updated breast cancer screening guidelines explicitly named DBT as the preferred modality for annual mammography. At this point in time, it is certainly reasonable to say that this technology is now considered the standard of care for both screening and diagnostic mammography.
However, despite the confirmed benefit and widespread acceptance of digital breast tomosynthesis, a gap exists between its utilization and its requirement for tomosynthesis-guided interventional procedures.
A New Challenge
While DBT has significantly improved mammography outcomes, it has also presented new challenges: detection of subtle, but definite areas of architectural distortion and amorphous calcifications seen only on tomosynthesis images without ultrasound correlates that they are not able to be confidently seen and biopsied using 2-D stereotactic biopsy systems. This has led to an increase in non-diagnostic procedures and the need for surgical excisional biopsies.
Thankfully, the introduction and availability of tomosynthesis-guided biopsy technologies has solved this critical problem — first utilizing add-on upright units and more recently with dedicated prone systems.
The advantage of add-on upright units is the ability to perform tomosynthesis-guided biopsies quickly and efficiently, increasing room functionality. However, they also have the distinct disadvantages of limiting capacity for diagnostic and screening exams, which may lead to backlog and vasovagal reactions, which are common with upright positioning.
A Case Study of Tomosynthesis-guided Prone Biopsy
New prone tomosynthesis-guided biopsy units now have all the advantages of 3-D localization — improved conspicuity of all lesions (including those only seen on tomosynthesis images), improved efficiency of procedures and lower radiation dose — with the added advantages of a dedicated procedure room to increase overall capacity and prone positioning to reduce concern of vasovagal reactions.
At Mills-Peninsula Women’s Center in California, we’ve found that our ability to perform tomosynthesis-guided prone biopsies has been integral to our reputation as a referral center for all breast procedures and a center of excellence for our patients. Thanks to this technology, we can perform challenging procedures quickly and efficiently.
Difficult Procedures
A recent patient referral to Mills-Peninsula illustrates this: A patient from an outside facility had a baseline screening mammogram detecting suspicious calcifications requiring biopsy, but with breast thickness of 18 mm, making a standard perpendicular approach with core needle biopsy impossible to perform. A surgical excisional biopsy was initially recommended. However, the surgeon referred the patient on to us at Mills-Peninsula, knowing we had the expertise and technology to perform this procedure for this patient.
What was impossible for another facility was now a straightforward and quick procedure thanks to the advancements of tomosynthesis-guided biopsy and the functionality of a lateral arm approach on the prone system.
Thanks to the lateral needle approach, access to parallel needle placement is available, quick and efficient. Essentially any lesion in the breast, even breast tissue that compresses very thin, is accessible for biopsy.
Patient Experience
Tomosynthesis-guided biopsies have had an enormous positive impact on patient experience. Procedures are now quickly and confidently performed because less imaging is needed, the field of view is larger and lesion conspicuity is increased. That means decreased procedure time for the patient with the breast in compression.
Previously, stereotactic biopsies could take 30-45 minutes to complete. This was a frustrating reality of older systems and technologies. However, thanks to newer biopsy technology, procedures can be completed in about 10 minutes.
In achieving this speed, one of the most important considerations is conspicuity of lesions. Whether it is calcifications, architectural distortion, round or irregular masses — if you can target on the first sweep of tomosynthesis images and see the lesion, then you can save a lot of time.
Another consideration is patient comfort. For many, prone systems offer a more compassionate, comfortable experience compared to their upright counterpart. That’s because direct view of the biopsy needle is eliminated with prone systems, helping to reduce worry of vasovagal reaction or other adverse responses.
Improved Workflow
Having a dedicated biopsy suite with a prone biopsy system improves workflow and capacity — something that is especially important at Mills-Peninsula due to our high volume and our patient commitment to have biopsy procedures performed within three days.
Upright biopsy systems decrease capacity for screening and diagnostic mammography, which may impact scheduling, leading to backlogs. For every biopsy conducted on an upright system, a facility loses scheduling for approximately four mammography procedures. This can have an especially negative impact, resulting in patient dissatisfaction, patient out-migration and lost revenue.
Having a prone system in a dedicated biopsy suite eliminates these concerns, allowing for more flexible scheduling, increased capacity for procedures and more efficient workflow.
Increased Capacity
Another benefit of the prone biopsy unit has been increased capacity for these needed procedures.
At Mills-Peninsula, we used to schedule a maximum of three stereos per day. Now we can perform three procedures in the morning and two in the afternoon. It is a real game changer for our facility.
Save the Biopsy Suite
Our experience with tomosynthesis-guided prone biopsy at Mills-Peninsula has solidified our commitment to this technology. While some may perceive benefits in transitioning to upright-only environments, we have experienced the benefits of tomosynthesis-guided prone biopsies at our breast center.
Truly, there is a case to be made to save the biopsy suite, and we have made it.
Harriet Borofsky, M.D., is the medical director of breast imaging with Mills-Peninsula Medical Center in San Meteo, Calif. She is a graduate of Harvard Medical School and completed her residency and fellowship at Stanford University Hospital, Calif.
Reference:
Adoption of Digital Breast Tomosynthesis in Clinical Practice, I. Richman et al, JAMA Intern Med., doi:10.1001/jamainternmed.2019.1058. Published online June 24, 2019. https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/…. Accessed Aug. 27, 2019.



 February 06, 2026
February 06, 2026 









