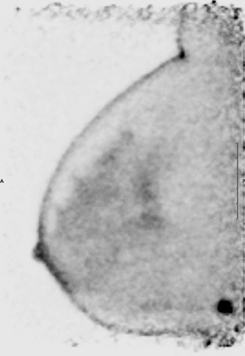
This image shows focal uptake suspicious for malignancy in the posterior breast near the chest wall.
Positron emission mammography (PEM) is an imaging technique designed to provide metabolic visualization of lesions in the breast tissue. The Naviscan high-resolution PEM system is a dual-detector system consisting of two flat, high-resolution detector heads using lutetium yttrium oxyorthosilicate in a 2 x 2 x 13 mm size. The detectors are mounted inside mammogram compression paddles with a 17 x 24 cm field of view. The paddles can be rotated to optimize imaging to match images acquired in standard mammograms. This allows for direct comparison with mammogram images.
Mammography uses X-rays through the breast tissue to make an image. Because of this, dense breast tissue presents a problem for diagnosis. A significant amount of the population has dense breasts. With PEM imaging, it does not matter if a woman has dense breasts or what stage she is in her menstrual cycle. Additionally, PEM is set for 10 to 15 pounds of pressure, which is significantly less than the 35 to 45 pounds of pressure required to obtain an adequate mammogram image.
The lesion size that is detectable with the PEM unit is as small as 1.6 mm, or the width of a grain of rice. Having the detectors so close to the breast tissue allows for an in-plane spatial resolution of 1.5 mm full width half maximum. This compares quite favorably to commercially available whole body positron emission tomography (PET) scanners that have a 4.2 to 6.5 mm axial resolution. Spatial resolution in a whole body PET scanner is also decreased due to respiratory motion, whereas with the breast immobilized in the PEM unit, there is no motion.
Mammography will always be the first line in detection of breast cancer. However, when mammography detects an abnormality, the patient then moves on to ultrasound and magnetic resonance imaging (MRI). A major disadvantage of ultrasound and MRI is their low specificity. Studies have shown that both the sensitivity and specificity of images produced by the Naviscan PEM scanner exceeds 90 percent. As a result, surgeons can more accurately stage lesions and plan surgeries, which can lead to fewer biopsies and post-lumpectomy re-excisions, and more breast conservation.
Three Years of Use Yields Positive Results
We have had our system at the Cancer Center of Santa Barbara for three years. The equipment is rather simple to use and the images are quite exquisite. In our experience, we have often changed the course of treatment for patients as we have detected satellite lesions that were not seen with any other imaging modality. There has been a slow acceptance of this technology in our area, but with more studies proving its value, we are seeing an increase in the ordering of this exam.
We have found patients tolerate PET mammography very well. We take four images that are eight minutes each (two of each breast). Due to the lengthy acquisitions, the patient is seated in a chair for imaging. This makes positioning more challenging for the technologist due to belly fat which is pushed upward against the bottom of the breast when seated. In traditional mammography the patient stands, which allows the belly fat to fall toward the pelvis and makes it easier to position the inferior paddle. There is a significant learning curve for the technologist for proper positioning of the breast. Additionally, lesions against the chest wall are difficult to image due to the dead space of the detectors.
Naviscan now has a biopsy device that attaches to the PEM unit, allowing image-guided core biopsies to be performed. This will aid physicians in obtaining tissue within the lesion that is “active,” providing more accurate biopsy results in lesions that are unclear on mammography, ultrasound or MRI. This biopsy can be performed in 15 to 20 minutes.
Various Agents Available for PEM
The PEM unit was specifically designed for high-resolution breast imaging with fluorodeoxyglucose (F-18-FDG). It is a molecule that is treated just as glucose in the body. The patient is injected intravenously with F-18-FDG, which goes to all the cells in the body. Tumor cells use more glucose than normal cells in the body. This phenomenon allows us to “see” tumor cells in the body with the appropriate equipment.
New drugs are being developed with the goal of imaging the biology of the cancer in each individual in the hope of targeting specific treatment for each person. This will enhance our knowledge of the tumors seen with this imaging modality, like the estrogen-receptor F-18 product (16a-[F-18]-?uoroestradiol-17b [FES]). This may provide an in vivo method of assessing estrogen receptors in primary and metastatic breast cancers and guide management with antiestrogen chemotherapy.
F-18 FLT ([F-18]-?uoro-L-thymidine [FLT]) is another drug showing promise. F-18 FLT is retained only in proliferating tissues. Every time a cell divides, it synthesizes its DNA to create a new cell. Thymidine is what is used to create the new DNA. By being able to image thymidine, we are able to see if the cells are growing or if growth is being slowed down due to therapy. [F-18]-?uoromisonidazole is a radiotracer marker for tumor hypoxia. With the advent of these drugs, it is a very exciting time for molecular imaging.
The future outlook of PEM imaging is fantastic. More facilities are acquiring this technology, which will move it into the mainstream of patient care.
Tricia Peters, CNMT, PET, is chief nuclear medicine technologist at the Cancer Center of Santa Barbara, Santa Barbara, Calif. She is a member of the Society of Nuclear Medicine and Molecular Imaging (SNMMI, formerly Society of Nuclear Medicine), Technologist Section.


 February 20, 2026
February 20, 2026 









