Patient X-ray radiation exposure from medical imaging has been a hot topic in radiology and has prompted the implementation of radiation dose monitoring systems. Prior to these systems, dose measurements either were not tracked or required manual calculation of dose based on scanner data in the DICOM headers. Since radiation doses per exam were often elusive, dose levels and scanning protocols vary, often greatly, between centers. Also, without automated dose tracking, no national standards have ever been established. Today, radiation dose tracking software is accumulating data at hospitals and in a nationwide dose reporting registry to help eventually set new standards.
The issue of dose monitoring came to the forefront a few years go after a couple reports in mainstream media on the extreme overexposure of patients to radiation doses during computed tomography (CT) exams at major hospitals on both the East and West Coasts. One of the biggest publicly reported incidents of radiation overexposure occurred in California in 2011. Due to improper settings on CT scanners, numerous patients received radiation burns and about 200 patients suffered hair loss, said Mahadevappa Mahesh, MS, Ph.D., chief physicist and professor of radiology and radiological science at Johns Hopkins Hospital, an expert in medical imaging radiation dose tracking. These incidents prompted California to pass a law now requiring radiologists to report the dose used in each exam. Texas also followed suit with similar legislation and other states are now considering their own versions of dose recording laws.
“The discussion about radiation dose has increased significantly over the past 10 years, and it is scaring a lot of patients,” Mahesh said. “This is partly because there is a lot of false information out there, and the mainstream media sometimes reports that medical imaging radiation can really cause harm. But it is helping on the other side in that it has changed the way we do imaging.”
In addition to changing laws in a couple states to require dose recording, public pressure from patients and mass media has led to a cultural change in many imaging departments. It also led to new dose recording requirements by the Joint Commission to maintain medical imaging certification.
How to Calculate Dose
There are several ways to calculate radiation dose measurement, and several different measurement units. Mahesh said this area is still evolving because there is no standardization. However, there are some common methods to collect data using the dose descriptor information automatically recorded by the imaging system and using multipliers to come up with an estimated, ballpark dose exposure. For example in CT imaging, dose parameters recorded by the scanners include CTDIvol and dose length product (DLP).
“These parameters are not patient dose, however, they are more like standard outputs for a particular technique, but they serve as a good estimator of patient dose,” Mahesh said.
He said it needs to be understood that estimates for dose using CTDIvol or DLP are based on ideal phantom model testing, using either a 32 cm water phantom to represent an average adult, or a 16 cm water phantom for an average pediatric patient. Mahesh said these are testing objects, not real people that come in all different shapes and sizes, and no patient is shaped like a cylinder. He stresses all dose measurements are ballpark estimates. Research into radiation dose is constantly changing based on new information. As new imaging technology becomes available and as the values for calculating dose change, he said it becomes complex to explain to patients or physicians why dose parameters for the same exam type and same patient changed between scans that are several years apart.
National Average for Medical Imaging
A big issue in medical imaging is that no national guidelines on standard doses have ever been established, so dose levels can vary significantly. “We saw a wide range in the protocols,” Mahesh explained. “That can result in the same person who gets a head CT at five different centers getting five different dose values. So we are trying to bring that gap in radiation doses much closer together.”
For this reason, Mahesh said there is a lot of effort being devoted to the American College of Radiology (ACR) Dose Index Registry. Hospitals can voluntarily sign up to participate in the registry and share anatomized patient dose information within the registry. In exchange, he said the hospitals can compare their dose averages for different protocols, type of exams and modalities used for hospitals in their area, or on a national level. “The idea is that eventually it will tell you where you are in these reference points so you can have an opportunity to refine and better manage your doses,” Mahesh said.
Dose levels have been dropping steadily over the past decade, but he said the pendulum has swung from one extreme of high dose to the other extreme of low dose. “At some of these extreme points of low dose, the images can get very hard to read or make a diagnosis,” Mahesh said. He suggests there should be some mechanism in the dose reporting quality assurance (QA) reports that note the diagnostic quality of the images. That way there can be a balance between the need to lower dose and a measure of the diagnostic quality of exams at specific dose ranges.
Need to Share Dose Reporting Data
At the end of the day, Mahesh said dose reporting analytics need to get into the hands of the radiologists and technologists, not just administrators or QA teams. “If administrators keep this information in a drawer and only pull it out for Joint Commission reviews, it is not serving its primary purpose,” he explained.
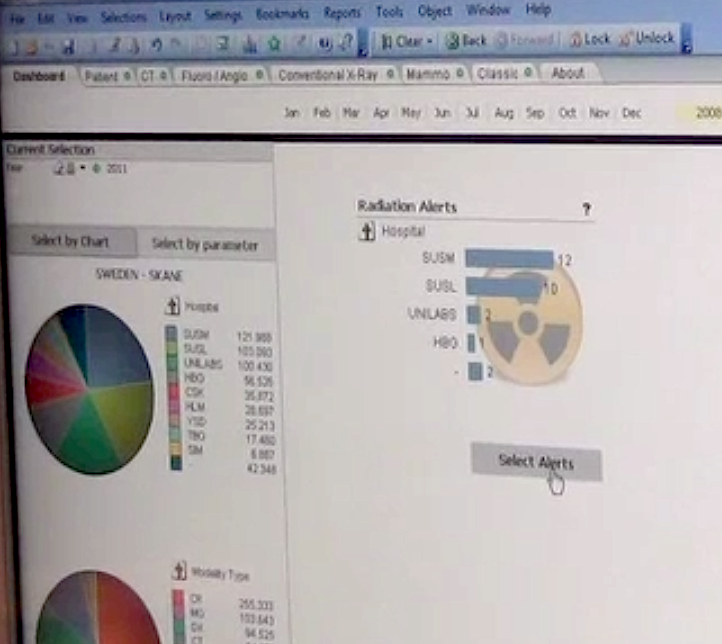
The human element is the weakest link in the chain for passing along key information in health informatics, including radiation dose statistics, said Paul Chang, M.D., FSIIM, professor of radiology, vice chair of radiology informatics, medical director of pathology informatics and enterprise imaging at the University of Chicago. During a health IT session at the Radiological Society of North American (RSNA) 2016 annual meeting, he said dashboards are often used by radiology administrators. However, dashboards often are not looked at unless the user is prompted by an alert or when they have a certification review. Unless the information can be shared with all the stakeholders involved in radiology, it is not effective and it will not affect change, Chang said. For this reason, he said use of automated reporting systems that make data available to all staff tends to be more helpful.
Mahesh said another issue with dose reporting data is interpretation, where a lot of radiologists and referring physicians might not understand what they are looking at. This includes not having a thorough understanding of how dose is calculated or what different dose levels mean for patient safety. Interpretation can also be a challenge if they see high-dose outliers, which could be due to the need for a retake exam because the patient moved and both exams were counted as one. A patient also might have a very high body mass index (BMI), which attenuates X-rays and requires high doses for diagnostic-quality exams.
The clinicians who have the most direct control over what dose is used in scans are the radiology technologists. They have traditionally been under pressure by radiologists to provide good quality, diagnostic images and to eliminate the need for retakes. This can result in techs upping the dose to create great quality images.
Comparison Chart for Radiation Dose Monitoring Systems
This article originally ran as an introduction to the Radiation Dose Management comparison chart in the September 2017 issue. The chart can be viewed here.


 February 04, 2026
February 04, 2026