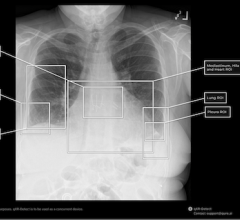
Photo courtesy of Carestream Health
Over the last decade, the field of medical imaging has evolved from analog technology toward the digital age. This shift in medical imaging has seen the emergence of flat panel detector (FPD) technology in everything from cardiology systems to portable X-ray equipment. Digital solutions have already begun to revolutionize medical imaging by offering improved image quality, faster processing time and dose reduction advantages over their analog predecessors. Those who have already adopted digital imaging are part of a market that continues to grow, expected to reach a sum of more than $35 billion by 2019.
Digital Evolution in General Radiology
For most facilities, the transition to digital occurred one system at a time. Cardiology and mammography departments, along with high-volume general radiography systems, were transitioned first as a result of the substantial improvements that digital offered. General radiography units are often saved for last or replaced on an ad hoc basis due to the larger inventory of equipment needing to be transitioned and the existence of computed radiography (CR) systems that allow images to be digitized.
Recently MD Buyline has seen an increased focus on converting these general radiographic systems including X-ray, radiography/fluoroscopy (R/F) units, portable X-ray and mobile C-arms to digital, flat-panel based technology. With these exams being the bread and butter of medical imaging — accounting for about 74 percent of the general radiologic exams performed in the United States — they play an important and vital role in the hospital, making their transition to digital a priority.1
System Pricing and Service Considerations
While digital has a lot to offer, understanding where this technology is needed most within a department and how to implement it in a fiscally responsible way can be daunting. When approaching the transition, it is important to determine when it is both cost-effective and clinically appropriate to incorporate digital technology.
The cost associated with digital technology for X-ray systems can be complex due to the number of system combinations possible and the option of the “digital retrofit” upgrade path. This allows use of an existing analog fixed X-ray or analog portable X-ray system by partnering it with a FPD in order to achieve direct digital technology in a cost effective manner. This option is especially important for facilities with analog units that still have several years of useful life remaining.
Price ranges for analog, retrofit and digital systems are provided in the chart to the right. There is also a considerable increase in cost of ownership related to service and support for digital systems. Facilities that previously paid $8,000–12,000 in annual maintenance fees for analog X-ray systems can expect to pay $30,000–55,000 per year for digital system service coverage. This is due in part to facilities electing for more full service agreements because of the difficulty associated with supporting a digital system, a lack of digitally trained biomedical engineer (BME) staff and “software keys” that are required to diagnose and repair the equipment. Notably, some vendors do not provide seamless access to software keys. This can force a provider into a comprehensive service agreement with that vendor.
Wireless detectors are an asset in today’s workflow because they are extremely portable. However there is also a greater risk of damage which leads to an increase in service costs. To avoid paying for a replacement panel at market price ($80,000–125,000), manufacturers offer separate drop-panel coverage by way of a deductible per occurrence ($5,000) along with an annual premium paid to offset the cost.
Clinical Considerations
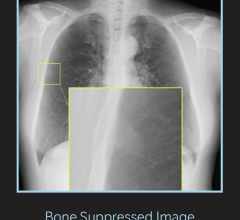
There are several clinical advantages associated with flat-panel based units, including higher image quality, less distortion, the potential for dose reduction and an immediate (within seconds) view of the image. When it comes to R/F systems, fluoroscopy units using dynamic detectors offer better penetration of anatomy, greater anatomical coverage area, more room within the system for patient positioning and a more sleek and inviting system appearance (detector components are less bulky than image intensifiers), which results in a less intimidating experience for patients.
Financial Considerations
There is no question that the cost of going digital requires a substantial investment and without any separate reimbursement for digital X-ray exams versus analog studies, it can be a difficult sell. However, there are some measureable soft dollar benefits that come with switching to digital and have the potential to offer meaningful savings.
Studies have found FPD systems can significantly improve workflow efficiency as compared to conventional CR systems.2 Due to this increased efficiency, a digital room can take the place of two or more analog rooms, freeing up valuable hospital real estate. Some of the newer digital systems include workflow and QA software that allows radiology administrators to track repeat exams and statistical trends usage of different technologist users. This tool is invaluable in helping departments identify opportunities to improve efficiency and image quality, provide additional training and education when necessary.
Using the latest digital, flat panel technology in mobile exam settings such as the ICU, OR and general hospital bedside gives the ordering physicians the ability to see an immediate view of the image at the bedside. Previously, technologists had to leave the area in order to process the images in a film darkroom or centralized CR reader. Instead of waiting 10–20 minutes for processing and image availability, physicians can now verify tube or line placement, make any needed adjustments and begin administration of medicines/nourishment in a much more efficient manner.
Employing digital systems in the medical imaging department can also help hospitals maintain the competitive edge with both patients and referring physicians. The information age is changing how patients seek out care. Patients are better informed about their options, such as the degree of technology available and the quality of care a provider can offer. As this trend continues and patients are more willing to choose their providers, hospitals will face the added challenge of competing for patients. This is a critical issue as volume is a key factor for the success of any service line. Furthermore, when referring physicians are aware that state-of-the-art digital technology is available at a certain facility, it breeds confidence in sending patients to that location, knowing that their imaging study takes less time, requires less dose and can be associated with higher image quality.
Prioritizing the Digital Transition
High volume areas such as the ER and outpatient X-ray rooms should be converted first. Specifically, determine where the improved turnaround and decreased wait time will have the most significant financial and customer service impact. When you are looking to prioritize, also consider patient volumes, types of exams that are performed and even the kinds of programs offered at your facility. For example if your hospital tends to perform the majority of the imaging exams for one or more local orthopedic practices, it would be appropriate to consider upgrading one or more outpatient imaging rooms to flat panel technology to ensure optimal efficiency and also gain higher image quality and detail that is needed to visualize fractures and bone pathology.
Another important consideration is if your organization offers a bariatric surgery program. These programs typically prefer sophisticated R/F systems equipped with a dynamic detector and higher table weight capacities. These system attributes also tend to be required for a Center of Excellence, Metabolic and Bariatric Surgery (COEMBS) designation as well.
Rooms used for hospital inpatients often rank lower on the list of transition, as workflow is generally slower in these areas, depending on the hospital’s size. Also for larger facilities or those that the department layout may involve X-ray systems that are located in other departments such as endoscopy or an older wing of the facility, there are many benefits to adding a boost in productivity to areas that are not centralized and need workflow efficiency improvements.
As many fluoroscopy exams, such as shoulder arthrograms, myelograms and intravenous pyelography, have been shifted to the advanced imaging modalities in the past few years, not all of a department’s R/F units may need to be converted to the latest digital technology immediately. In general, most hospitals have found that lower volume radiology, R/F rooms and mobile C-arms — depending on the demand by surgeons — can be converted last as well.
When approaching the transition, move earlier generation digital systems to facilities and clinics within your network with lower volumes if there is still plenty of life left on these units. Review service records and your equipment inventory with clinical engineering, BME and your service/support provider to obtain an idea of the age, repair and downtime history of older systems. Review computed radiography (CR) systems, imaging plate and cassette condition as well as the recent repair trending for these units. If you have experienced increased downtime with CR readers or need to replace a large number of imaging plates, it may be worthwhile to compare these costs to an investment in FPD technology. Always replace the oldest and problem units first to avoid pouring more service and support money into lost causes.
When and Where Analog Is Still Appropriate
The continued use of CR, which has served as a bridge from analog to digital by providing digitized images that can be sent to PACS, will continue to be a viable option in low-volume scenarios where slightly longer processing times and consequently longer exam times for patients do not adversely affect the department’s workflow. Rural hospitals and clinics, as well as physicians’ offices, will most likely continue to utilize CR until it is feasible both financially and from a productivity standpoint to make a change. In addition, for those facilities that may have strict budgetary controls in place or have exhausted their technology upgrade budget, CR and image intensifier based systems can continue to be legitimate levels of technology in today’s radiology departments, as long as they can push digitized images to PACS and the EMR.
Future Outlook
It is imperative that general radiology does not get left behind as the rest of the world moves digital. It can be easy to overlook the impact and importance of general radiology on patient volumes and consequently, the bottom line, as reimbursements are much lower for these types of exams and especially due to the high cost associated with upgrading technology. However, the clinical benefits and soft dollar considerations can help offset some of the financial burden. Even though the high price of going digital presents a challenge in today’s healthcare economy, it will not be long until we are looking at analog technology as a thing of the past.
Digital X-ray Systems Comparison Chart
ITN has created a comparison chart for specifications for digital radiography systems, both fixed and mobile. It can be accessed at www.itnonline.com/content/digital-radiography-systems. This will require a login, but it is free and only takes a minute to register. The chart includes all manufacturers of mobile C-arms that sell systems in the United States.
Related Articles on the Transition to Digitital Radiography
Digital Radiography Facing Major Change in 2017
Mobile Digital Radiography Driving Efficiency
CR to DR: The Time-Saving Solution for a Critical Access Hospital in New Hampshire
An Effective Approach to X-ray Equipment Upgrade
VIDEO: Technology Report: DR Systems
Lori Webb joined MD Buyline in 2008 with an extensive 20-year background in radiology. She continues to practice as a clinician in her spare time at a local emergency facility. At MD Buyline, she assists hospitals and healthcare facilities with purchasing considerations, product research and comparisons on analog and digital radiographic equipment, radiology IT systems. She is also registered by the American Registry of Radiologic Technologists.
Katie Regan joined MD Buyline in 2013, bringing with her seven years of clinical research experience. At MD Buyline, Regan is responsible for all clinical, financial and general healthcare publishing projects. Her work has been published in hfm Magazine, Becker’s Hospital Review, ITN and DOTmed. She currently serves as a member of the DOTmed HealthCare Business News Editorial Advisory Board.
References:
1. www.asrt.org/docs/whitepapers/asrt12_bstpracdigradwhp_final.pdf. Accessed Sept. 5, 2014.
2. www.ajronline.org/doi/full/10.2214/AJR.10.5867. Accessed Sept. 5, 2014.


 March 03, 2026
March 03, 2026