Since the advent of ultrasound scanning in the 1950s, the global movement to develop and expand its diagnostic features continue in its appeal with the medical community today. The ultrasound design using sound waves and echo reflection became widely accepted for being the safe (non-radiation), inexpensive, repeatable and non-invasive alternative in medical imaging. Early clinical upgrades included the development of the pulse Doppler paradigm (1966) to enable scanning layers of the heart via blood flow. This offered diagnostic advantages to its application in the mid-seventies for live-action scans of the human fetus. These qualities earned its place as the standard in pediatric use while continuing to earn the confidence of radiologists and imaging specialists for a wide range of diagnostic applications, from emergency critical care to supplemental cancer screening.
The Science of Blood Flow and Doppler Technology
Hemodynamics is defined as the study of blood flow in relation to the status of the circulatory system and autoregulation. Monitoring the blood flow can provide many answers to the health and physiology of the target area scanned as well as cell-level metabolism, the regulation of the pH, osmotic pressure and temperature of the whole body, as well as any effects from foreign influences.1 Evaluating injuries, inflammation or mutative growths (including cancer tumors) through the assessment of blood flow offers quantitative information about the status of tissue disorders or tumor malignancy.
According to cancer diagnostic imaging expert Robert L. Bard, M.D. DABR, FASL, the introduction of 4-D Doppler technology aligned with the ultrasound’s base design concept of providing instantaneous, real-time readings. “Let’s take the case of breast cancer screening. The technician simply puts the probe on the breast, finds the area, pinpoints it, presses a button and seconds later you have the map showing the types of vessels, volumetric arterial density and spatial location of the vessels in relation to the adjacent organs,” he explained. “You have functions that give you a vessel density measurement, which shows how aggressive this is. Instead of genetic markers (which are very popular), visually displaying tumor aggression performed in a matter of seconds to show cancer vessel invasion is a game-changer for any early detection or monitoring facility. Tumor aggression by blood flow evaluation is used worldwide in nuclear medicine, computed tomography (CT) scans and magnetic resonance imaging (MRI) technology, however, one of the simplest and most cost-effective alternatives is the non‐invasive 3-D Doppler breast procedure.”
Intracranial Scanning With Doppler Ultrasound
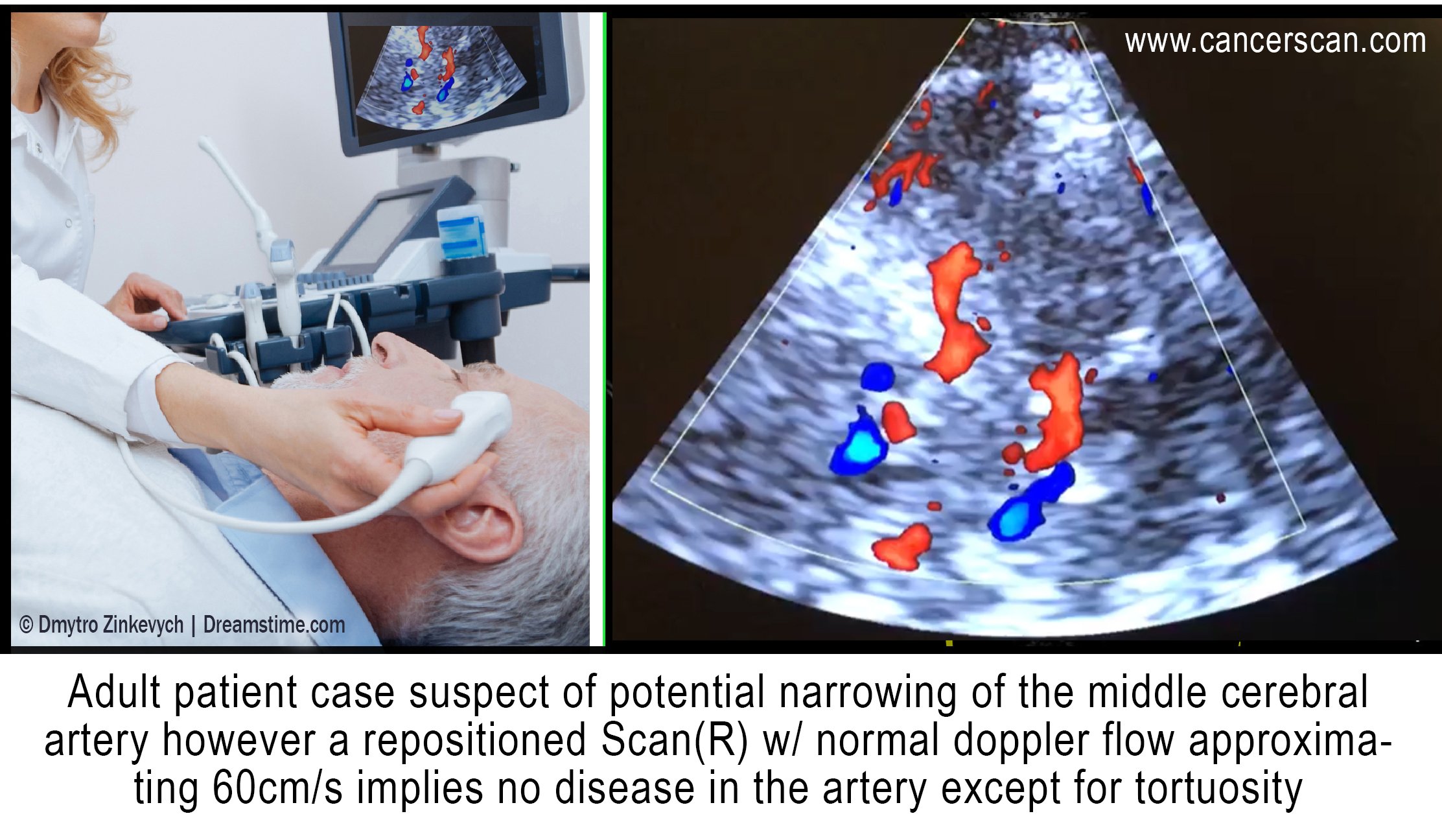
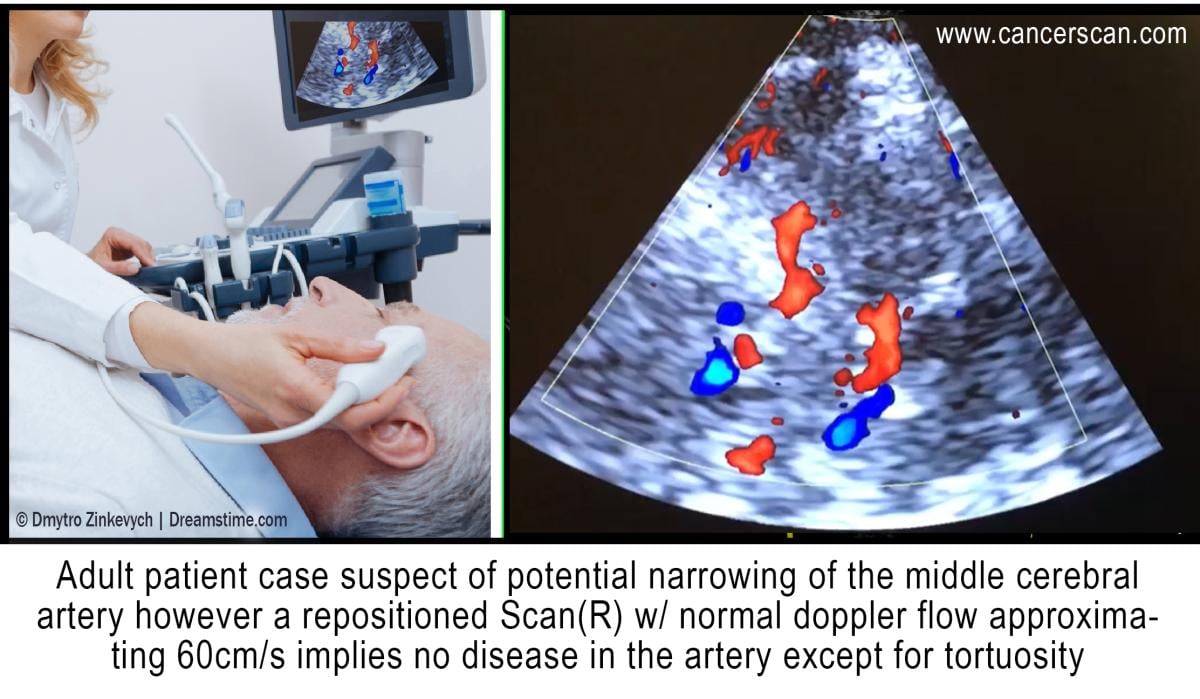
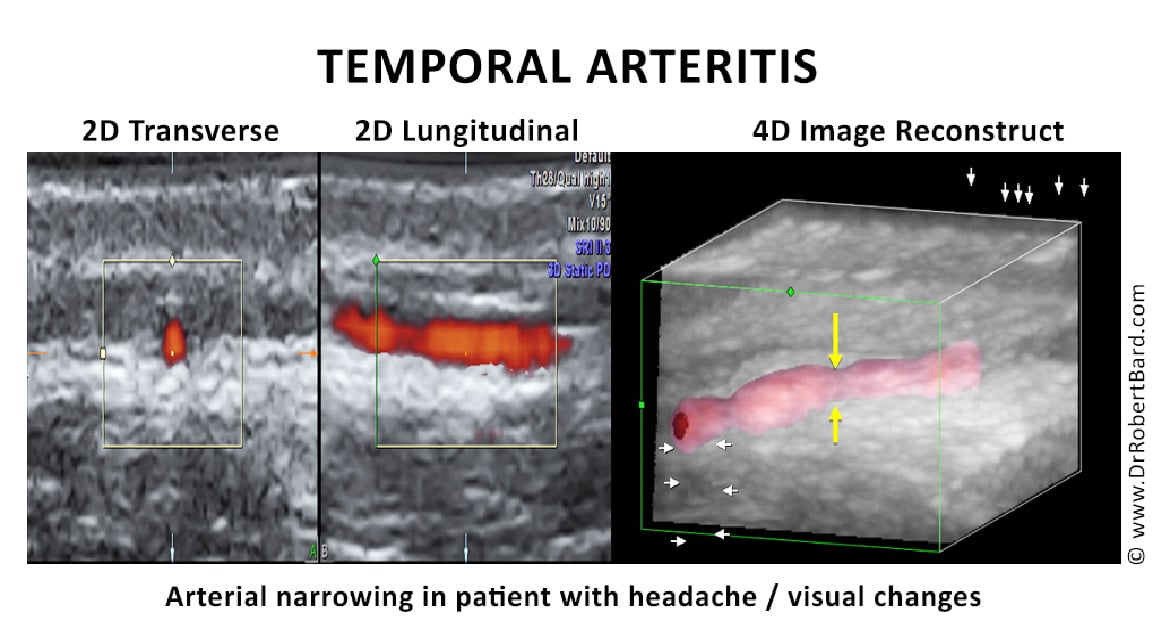
In 1982, continued advancement led to the Transcranial Doppler (TCD) ultrasonography for outpatient and inpatient settings. By integrating the ability to study blood flow with a low-frequency transducer, placing the probe on the temporal area measures the cerebral arteries to detect and quantify cerebrovascular activities, diseases and brain injuries. Other applications include the diagnoses of vasospasm (VSP) after an aneurysm rupture, hemorrhage or hemodynamic changes after ischemic or cryptogenic stroke. It also enables the study of cranial pressure fluctuations.
TCD imaging also offers significant clinical benefits in the monitoring of sickle-cell disease by scanning brain stem death and elevated raised intracranial pressure (ICP). Added features allow for surgical and post-op monitoring of vasomotor functions as well as detecting critical disorders like a microembolism.2
part 2
Verifying Signs of COVID-19 Stroke Through Imaging
By Robert L. Bard, M.D. DABR, FASL, and Pierre Kory, M.D.
Early detection and prevention of arterial and venous disease is key to minimizing the effects of arterial obstruction and hemorrhage, brain aneurysms and strokes from venous thrombosis. The association of trauma to PTSD is now followed by advanced Doppler ultrasound and functional MRI. This abnormal physiology may also manifest as arterial dissection, collagen disease, inflammatory arthritis, dermatitis, ocular disorders, GI disturbances, limb pain, or aneurysms of the brain and aorta. Devastating strokes in the COVID-19 era occur in the younger age group and the Latin population who are at higher risk.
Introduction to Arteritis
Interest in arteritis was elevated with the study of Tayakasu’s disease in the 1970s when advances in contrast arteriography diagnosed diffuse vascular involvement causing strokes and aneurysms in multiple sites. While this arterial inflammation is more common in Asians, in the U.S., blacks are nearly three times more likely to have a stroke at age 45 than whites. The pediatric population seems to be at higher risk for this arteritis as evidenced by their unusual rate of COVID-19 affliction affecting the vasculature and called Multiple Acute Inflammatory Syndrome in Children (MIS-C). Birth control pills are a distinct cause of such disease in younger women, while cancer, alcoholism and obesity raise the incidence at all ages.3
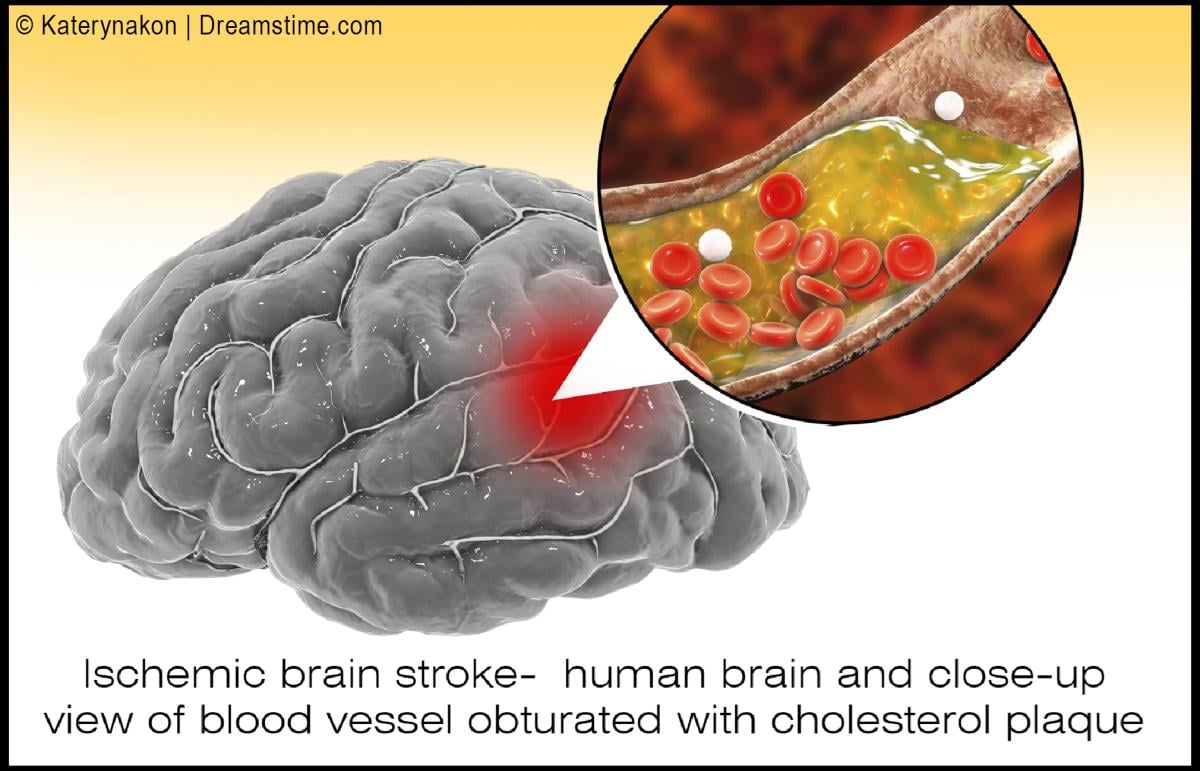
We have learned over the last century that blockages of coronary arteries to the heart and carotid arteries to the brain are precipitated by inflammation of the inner walls of the vessel, called the intima.
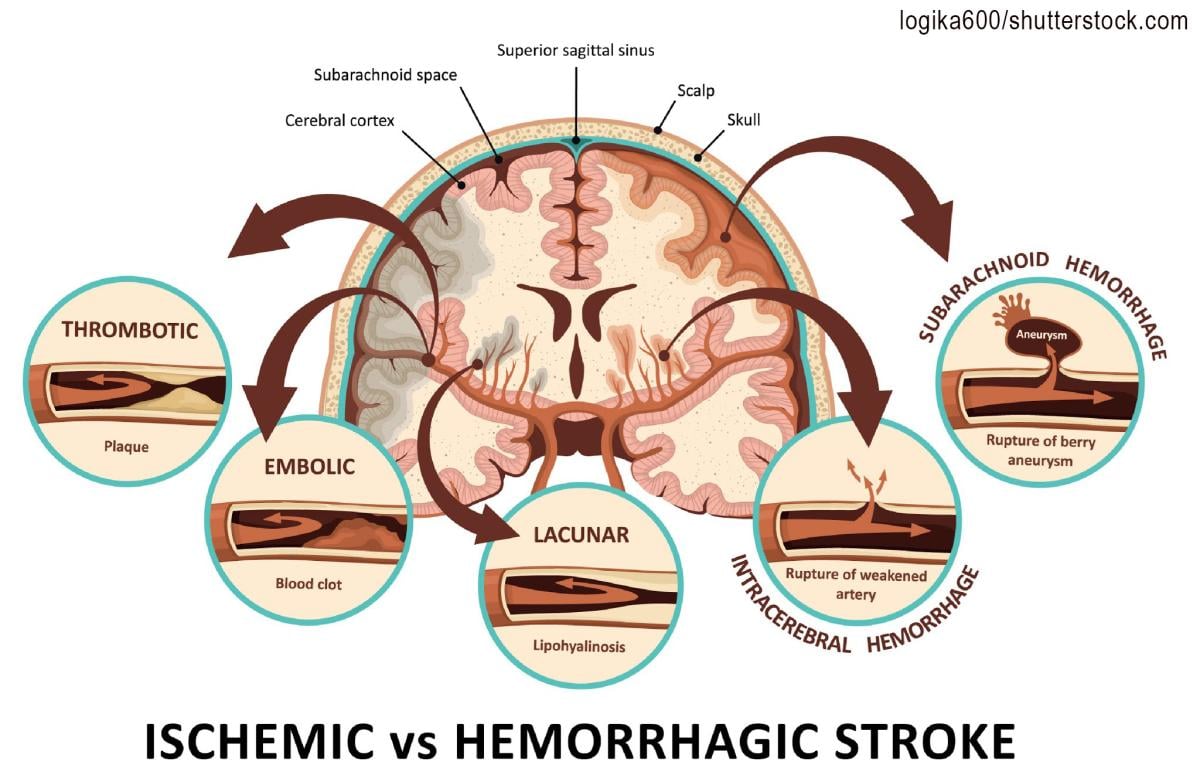
While thickening of the interior wall of vessels gradually occurs over time and is aggravated by diet, stress and hypertension (high blood pressure), the acutely disabling event occurs when there is an abrupt tear of the overlying plaque that ruptures debris, which then forms a blood clot that blocks blood flow, or the clot travels deeper into the brain and blocks blood flow. Similarly, abnormal heart rhythms such as atrial fibrillation causes the pooling of blood in the heart, which predisposes to clot formation, and the clots can then travel into the brain causing a stroke. In COVID-19, the virus causing severe inflammation in the blood then promotes clot formation that can travel through the vascular system and affect almost every organ system in the human body, with the brain and lungs being the most vulnerable. An article in September 2021 Neurology reported by Medscape documented the incidence of large artery stroke as the presenting symptom of COVID-19 was highest in men under the age of 50 years.4
History of Arteritis
A medical research team at Metropolitan Hospital in New York first noticed unusual neurologic symptoms in young and middle-aged patients in the late 1960s. As a division of the NY Medical College system, they were fortunate to have an active interventional radiology department specializing in neuroimaging and arteriography. The observation of distortion and occlusion of arteries supplying the brain, kidneys, GI tract and lower limbs to various degrees from single to multiple locations was closely linked to the Japanese disorder known as Tayakasu’s arteritis at the time and recently renamed “arteritis.” A clinical finding of this arterial inflammation in the abdominal aorta was pain in the upper abdomen near the great vessels by palpation. Astute physicians were successfully treating this with commonly available aspirin.
However, the chronic and diffuse nature of arteritis often weakened the vessel wall, producing aneurysmal dilation and rupture. Today we find sophisticated non-invasive or minimally invasive modalities to be the first line of interrogation of vasculitis.5
COVID and Stroke
COVID-19 was rapidly understood as a disease caused by severe and widespread inflammation and “hypercoagulability” (a tendency to spontaneously form clots in the blood vessels). Autopsies have revealed extensive small vessel strokes, with such strokes often occurring despite aggressive blood thinner treatment and regardless of the timing of the disease course, suggesting that it plays a role very early in the disease process. In one autopsy series, there was a widespread presence of small clots with acute stroke observed in over 25%. In a recent review of the incidence of stroke in COVID-19, almost 2% of all hospital patients suffered a stroke, which is eight times higher than in patients with influenza. More worrisome is that this is almost definitely a gross underestimate given the many likely missed strokes in patients who died on ventilators who were too ill to obtain imaging, the general restrictions on and lack of autopsies, and the well-recognized decrease in the number of patients with acute stroke symptoms seeking medical attention in the COVID-19 era. Another worrisome finding from a recent study of COVID-19 cases found that 45.5% of patients reported neurologic symptoms.6,7 This under-recognized epidemic of neurological symptoms and strokes in COVID-19 highlights the need for more intensive imaging and investigation to achieve not only earlier recognition and improved treatment of patients, but in furthering understanding of COVID-19 effects on brain function.
Diagnosis by Imaging
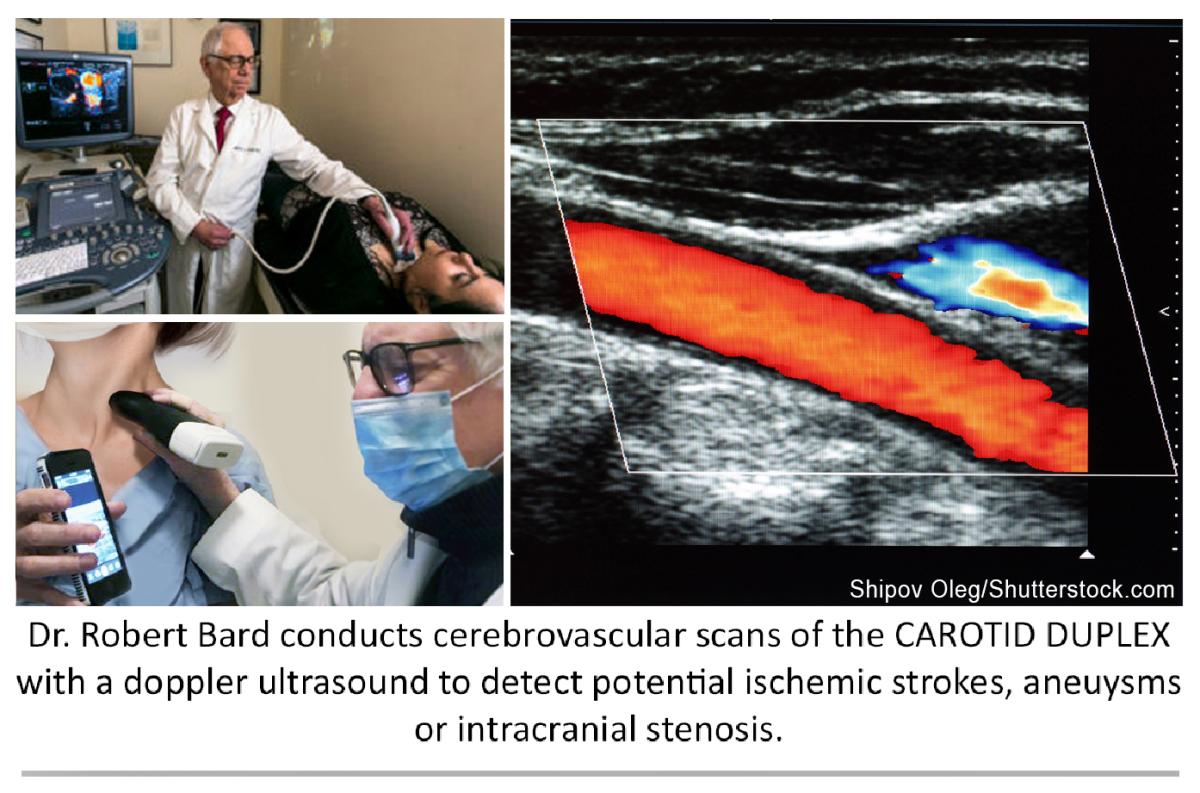
Blood flow abnormalities in the arterial system are best studied by Doppler imaging like the weather Doppler showing tornadoes. Multiple options exist for blood flow analysis including:
• Carotid sonogram
• Carotid Doppler
• Eye sonography
• Transorbital Doppler
• Contrast enhanced ultrasound
• Transcranial Doppler imaging
• Hybrid imaging
• 3-D/4-D vessel density histogram
• Endoarterial 3-D Doppler
• Retinal OCT
• Soft tissue OCT
• Reflectance confocal microscopy
• Small coil MRI
• 7 Tesla MRI
Carotid Sonogram
While cerebrovascular disease is often diagnosed ex post facto after a catastrophic episode with MRI and CT, the non-invasive Doppler analysis of the vascularity is generally checked with ultrasound for plaque and obstruction. A useful measure of the risk of coronary and cerebrovascular disorder is the carotid intimal thickness (CIMT). Standard depth of the inner wall thickness is a measure best obtained by high resolution sonograms since a reading over 0.9 mm indicates increased risk. The newer sonogram units have depth resolution of 0.02 mm making this a preferred non-invasive option.
Sidebar:
Doppler Imaging Technologies
Color Doppler — most common application where red is flow towards the probe and blue is flow away from the probe.
Power Doppler — higher spatial resolution without directional flow correlation.
3-D Power Doppler — allows volumetric analysis of vessel density used in treatment correlation where more vessels mean increased neovascularity and fewer vessels correlates with clinical improvement.
Angio Doppler — similar to color Doppler with higher spatial resolution.
Microvascular Doppler — images capillary flow.
B-Flow Doppler — not true flow technology, but observes motion of red blood cells directly.
Carotid Doppler — flow abnormalities of turbulence and absence are commonly evaluated with this modality. Plaque forms more readily in aberrant flow patterns and high velocity regions accompanying narrowing.
Eye Sonography — sonofluoroscopy of the orbital soft tissues and eyes is performed in multiple scan planes with varying transducer configurations and frequencies. Power and color Doppler use angle 0 and PRF at 0.9 at the optic nerve head. 3-D imaging of optic nerve and carotid, central retinal arteries and superficial posterior ciliary arteries performed in erect position before and after verbal communication. Retinal arterial flow is measured. Optic nerve head bulging is checked as increased intracranial pressure may be demonstrable.
Transorbital Doppler —R/L ciliary arteries have normal Doppler flows of 10 cm/s, which is symmetric.
Contrast Enhanced Ultrasound — widely used European nonionic contrast injection allows imaging of the capillary vessel sizes and
perfusion characteristics.
Transcranial Doppler Imaging — this measures the flow
in the anterior, middle and posterior cerebral arteries as well as
Circle of Willis.
3-D/4-D Vessel Density Histogram — multiple image restoration and reconstruction shows retinal vessel density of 25% at the optic nerve head and adjacent region with quantitative accuracy.8
Endoarterial 3-D Doppler — microcatheters inserted into the arterial or venous system provide measurement of wall thickness and presence of inflammatory vessels inside the intima.
Retinal OCT — subtraction techniques done with optical coherence tomography (OCT) may show changes in the caliber of the retinal vessels with verbal ideation.
Soft Tissue OCT — the depth of penetration may be extended to 2-3 mm allowing for analysis of vascular changes in erythematous or erythropoor dermal areas. Thrombosis may be observed.
Reflectance Confocal Microscopy — this microscopic analysis of the cells also quantifies microvascular pathology and is a potential modality for studying vasculitis.
Small Coil MRI — high-resolution systems used for animal study and superficial organs can image the intra-arterial anatomy, including dynamic contrast imaging on standard 1.5T and 3T units.
7 Tesla MRI — High-field systems analyze signal abnormalities rapidly with high resolution.
Hybrid Imaging — hybrid imaging refers to combining diagnostic modalities to assess disease and monitor therapy.

Lennard M. Gettz, Ed.D., is research director of the NY Cancer Resource Alliance educational initiatives, founder of the Integrative Pain Healers Group and VP/executive director for the First Responders Health Advocacy of the FACES Foundation (Firefighters Against Cancer & Exposures). He is also the producer of the AngioFoundation (501c3) “Med-Tech Reviews” video series.

Noelle L. Cutter, Ph.D., is Interim associate dean at Molloy College, professor of biology and chemistry, cancer researcher on immunology and treatment options for medulloblastoma (pediatric brain cancer). She is also an “Iron-Man” race winner and dedicated triathlete.
Robert L. Bard, M.D., PC, DABR, FASLMS, is active medical director of Cancer Diagnostic Imaging Center (NYC), using advanced 3-D ultrasonographic Doppler imaging to detect cancers in breast, prostate, skin, thyroid, melanoma and other areas. He has extensive credentials as a clinical researcher/validator and has published medical textbooks and science journals.

Pierre Kory, M.D., is a critical care physician who gained attention during the COVID-19 pandemic for advocating widespread off-label use of certain drugs as treatments for COVID-19, as president and co-founder of the Front Line COVID-19 Critical Care Alliance.
References:
1. Hemodynamics: https://en.wikipedia.org/wiki/Hemodynamics. Accessed Jan. 3, 2022.
2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5224659/. Accessed Jan. 3, 2022.
3. Hassani SN, Bard RL: Ultrasonic Diagnosis of Aortic Aneurysms. J. Natl. Med. Assoc. 66:298-299, July 1974
4. Lande A, Bard RL: Arteriography of Pedunculated Splenic Cysts. Angiology 25:617-621, October 1974
5. Lande A, Bard RL, Rossi P: Takayasu’s Arteritis: A World Entity. N.Y. State J. Med. 76:1477-1482, Sep 1976
6. Helbick Eur Radiol 30:5536-5538, 2020
7. Mao l JAMA Neurol 2020 77:683-690
8. Bard RL , Gettz L, van der Bent S etal: Proceedings of the 4th Inflammatory Disease Summit at NY Academy of Medicine Nov 2021
Related Content:
Stroke Scans Could Reveal COVID-19 Infection
Lung Scans for Stroke Patients Could Provide Earlier COVID-19 Detection
PHOTO GALLERY: How COVID-19 Appears on Medical Imaging
Digital Health Devices Used at Point of Care May Improve Diagnostic Certainty



 February 05, 2026
February 05, 2026