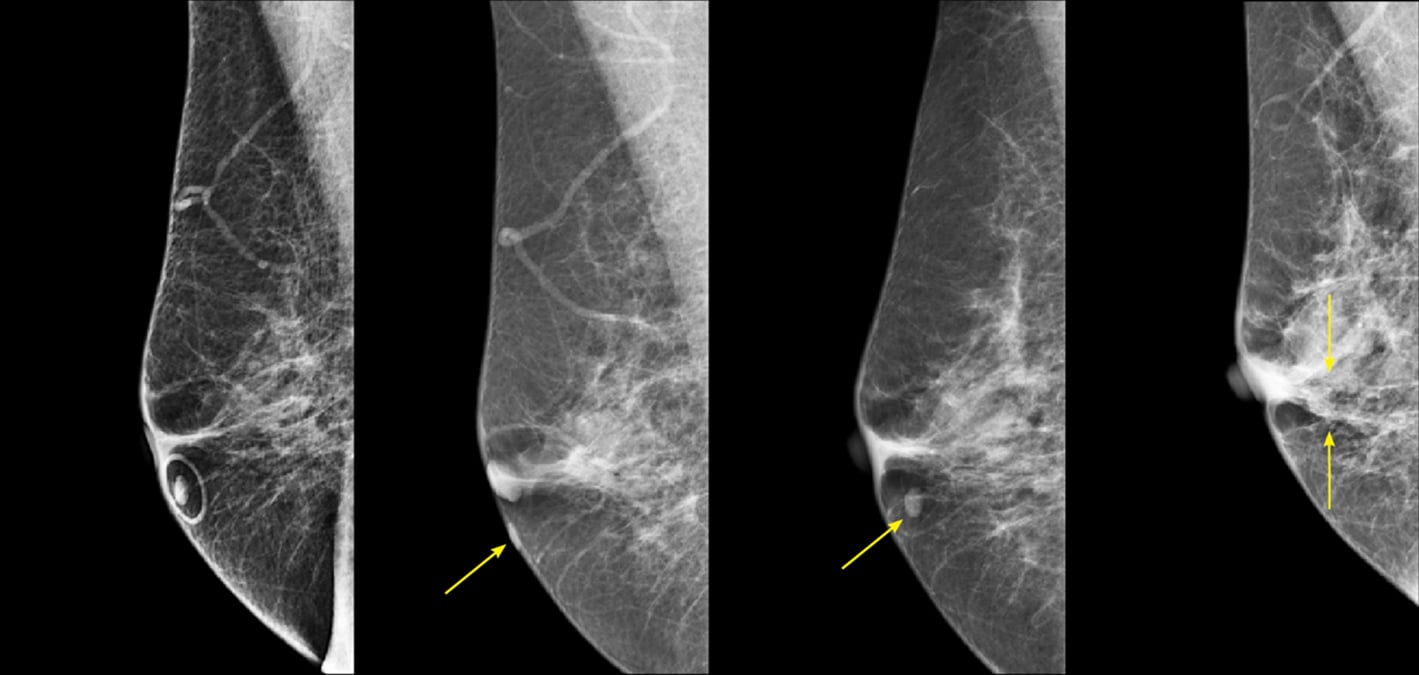
Figure 1. R MLO view from four different years. The skin mole is marked with a circular skin marker (TomoSPOT REF# 782, Beekley Medical) on the far-left image. These images demonstrate the potential for significant variability in location of the skin lesion due to movability of the skin during positioning.
Christina Jacobs, M.D., Director of Breast Imaging (Bronson Health System) is always looking for ways to work more efficiently and improve the patient experience. She found that using skin markers not only facilitates the radiologist’s interpretation and improves workflow, it also helps reduce avoidable patient callbacks
and increases standardization across exams.
At her institution, she uses markers with specific shapes to designate different areas of clinical concern such as palpable lumps, areas of pain or concern, scars, and moles or other skin lesions. This is in accordance with recent guidelines issued by the American College of Radiology (ACR).1
Mammograms at Bronson Health are performed under both 2-D full field digital mammography (FFDM) and 3-D mammography or digital breast tomosynthesis (DBT). Jacobs prefers skin markers designed specifically for DBT as they generate less artifact.
Moles Pose an Interpretation Challenge in DBT
While variation in equipment, technique, patient positioning and anatomy are commonplace in all mammography, DBT poses a unique set of challenges in identifying skin lesions compared to traditional 2-D digital mammography.
According to Jacobs, using mole markers in DBT is helpful to address these challenges.
• Some manufacturer’s equipment may add five extra reconstructed slices to the compression paddle side to eliminate the possibility of displaying the breast incompletely, thus causing a skin lesion to not appear on the initial slices. This means that in small breasts, lesions will appear to localize closer to the detector side of the scroll bar.1
• In addition, if the paddle flexes, an anterior skin lesion will be on a deeper slice because the breast is thickest at the chest wall.2 A skin lesion may not appear on the initial slices when the lesion is on a curved surface of the breast that is not in contact with the detector or compression plate.
• Rolling of the breast on the orthogonal view can change apparent skin lesion location and mislead the radiologist.3 In larger breasts, the craniocaudal (CC) view is more susceptible to this rolling of superficial tissue.4
“This variation can result in things not being where you expect them to be on one view versus another,” Jacobs stated. “This can be especially true for superficial skin lesions in women whose breast tissue is pliable and stretches more. The way the tissue is spread out by the technologist also makes a difference. Moles that are closer to the chest wall where the tissue is less mobile tend to be more consistent and have less variation in their image location from view to view.”
Moles which are further out on the breast can be represented in significantly different locations as shown in Figure 1.
If a skin lesion is in the lateral portion of the breast, the true lesion location will be inferior to what is shown on the mediolateral oblique (MLO) view. If the skin lesion is in the medial breast, the lesion will be superior to what is shown on the MLO view.2
Mole Markers Reduce Avoidable Callbacks
To further emphasize how mole markers clarify findings and improve interpretation, Figure 2 shows a L CC view with a circular marker denoting a skin mole. Figure 3 shows the corresponding MLO view. The retroareolar asymmetry on the CC view would not be as obvious as corresponding to the skin lesion on the MLO view without the mole marker.
“If the mole marker had not been used,” Jacobs explained, “this patient would have been called back for additional views. Having the skin marker lets you correlate with 100 percent certainty that it is the same finding on the two views.”
Improved Communication and Workflow
Having a protocol for the use of skin markers decreases the chance of misinterpretation and improves communication between the technologists and the radiologists.
Jacobs recalled a case where a potential mass was identified on the CC view of a patient who was imaged without any markers. When the patient returned for additional imaging, the technologist noticed a mole in the area of concern and marked it with a circular mole marker, confirming that the suspected lesion was a skin mole and not a mass.
“When our technologists use markers with specific shapes to indicate specific areas of concern it makes our workflow more efficient,” Jacobs stated. “When I’m reading an exam with skin markers, I know what each shape means. This facilitates efficient interpretation and reduces the need to review technologist’s notes on prior exams. It saves time, decreases callbacks, and makes it safer for the patient.”
Breast Maps Alone Are Not Sufficient
Jacobs believes skin markers to be a more accurate documentation of the patient’s intake history than charting alone.
“Our technologists are required to note the area of interest or concern on the breast map in our electronic reporting system. However, the drawing is just a mock-up and is not exactly what you see on the CC and MLO views. Patients have variability in their breast size and pliability of the breast tissue that can affect location on the image. It doesn’t always match the drawing, and the breast map doesn’t always correspond with where an area might end up on the actual image. It leaves room for potential misinterpretation.
“Using skin markers has been very beneficial for our practice,” Jacobs continued. “They improve efficiency, workflow of our radiologists and improves communication between the technologists and radiologists.
“For the patient, reducing callbacks means we can minimize inconvenience, anxiety, and additional radiation exposure. It makes the overall experience that much better for our patients,” she concluded.
For more information: www.beekley.com
References:
1 The American College of Radiology, ACR BI-RADS® Atlas – Mammography, Digital Breast Tomosynthesis (DBT) Guidance, (A supplement to ACR BI-RADS® Mammography 2013), retrieved from https://www.acr.org/-/media/ACR/Files/RADS/BI-RADS/BI-RADS-Digital-Breast-Tomosynthesis-Supplement.pdf.
2 Ibid.
3 Lesion localization using the scroll bar on tomosynthesis: Why doesn’t it always work?, Friedewald, Sarah M. et al., Clinical Imaging, Volume 47, 57 - 64.
4 Ibid.




 March 06, 2026
March 06, 2026 









