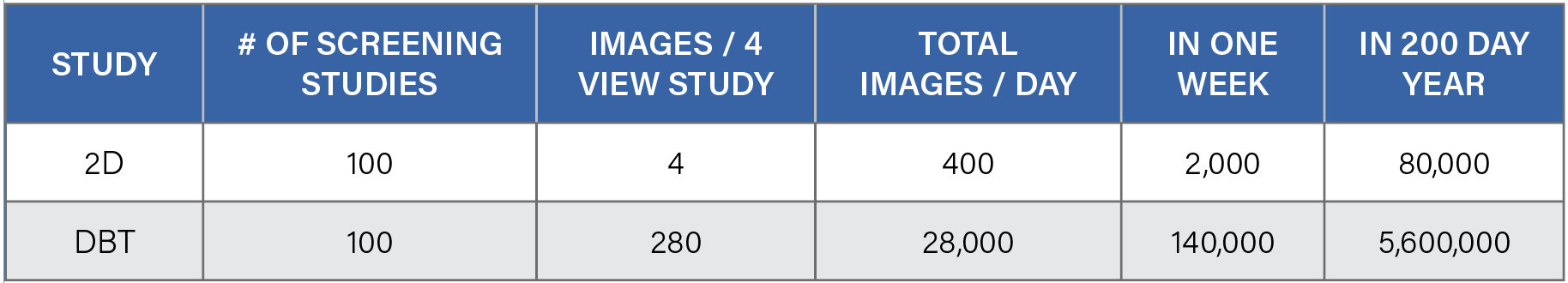
Table 1. Compared to 2-D mammography, which yields four images per patient, digital breast tomosynthesis (DBT), or 3-D mammography, produces hundreds of images per patient. While this provides more information for clinicians, the exponential increase in data can result in reader fatigue and burnout, which may ultimately affect patient care.
As the largest independent imaging group in Michigan with 10 locations across the state, Regional Medical Imaging (RMI) has been providing superior imaging services for 35 years. Co-owner and CEO, Randy Hicks, M.D., MBA, provides both a clinical and pragmatic approach to running the business, which has led RMI to become one of the leading radiology facilities in the state, with a team of experts in women’s imaging and other subspecialties.
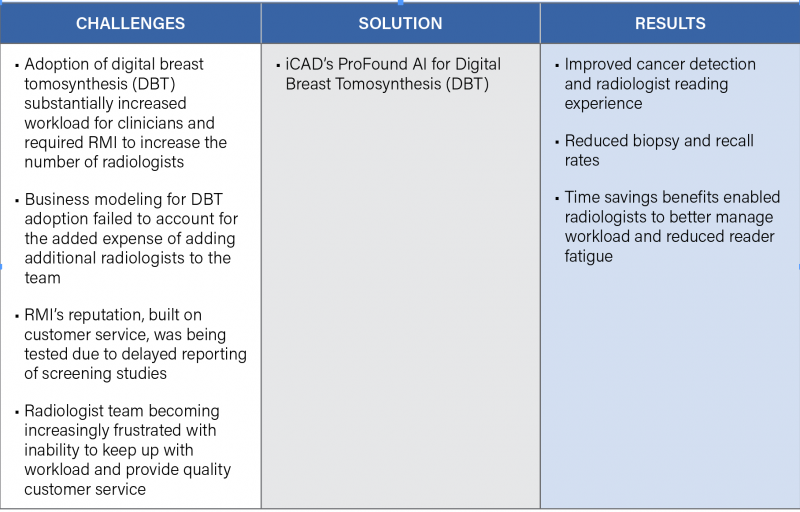
Hicks takes pride in ensuring that RMI features the latest in state-of-the-art technology that empowers his team to provide the best possible patient care. In 2018, RMI adopted DBT systems across all 10 of its locations. But while digital breast tomosynthesis (DBT), also known as 3-D mammography, offers a number of benefits to patients, such as enhanced breast cancer detection and fewer false positives and unnecessary recalls, it produces hundreds of images per patient, compared to 2-D mammography which typically only produces four images per patient.
“We were starting to feel like we were on the Titanic. The exponential increase of images quickly began to take its toll on the team,” Hicks said. “Mammograms can be anxiety inducing for women, and ultimately they just want the report that says negative. With the increased workload from DBT we were taking longer to get those results to our patients. We needed a solution to manage this workload, and we needed it badly. The minute ProFound AI was FDA-cleared, we knew we had to have it at RMI.”
In December 2018, ProFound AI for DBT became the first and only software for DBT with artificial intelligence (AI) to be FDA-cleared. Designed to be used concurrently by radiologists reading 3-D mammography, the technology was trained with the latest in deep-learning AI to detect malignant soft tissue densities and calcifications with unrivaled accuracy. It is the only software of its kind that rapidly and accurately analyzes each DBT image, or slice, and provides radiologists with crucial information, such as Certainty of Finding lesion and Case Scores, which can assist in clinical decision-making and prioritizing caseloads.
Positive clinical results from a large reader study were recently published in Radiology: Artificial Intelligence. In a large reader study, ProFound AI for DBT increased radiologists’ sensitivity by 8 percent, minimized the rate of false positives and unnecessary recalls by 7 percent, and reduced reading time for radiologists by 52.7 percent.1
The Paradigm Shift
Upon implementation of ProFound AI, the team at RMI immediately began to experience a number of benefits, including improved cancer detection, a reduction in biopsy rates and a reduction in unnecessary recalls. Reading time for radiologists was also substantially reduced — and the team at RMI found ProFound AI to be even more reliable than expected.
“The paradigm really shifts when you get ProFound AI — it changes the way you read. Once you use it, it’s really quite shocking how impressive it is,” said Hicks. “The technology itself is better than humans. Once we started using ProFound AI, we realized we are finding more cancers,” Hicks stated. “It takes time to trust it — but believe me, you can trust it. ProFound AI definitely finds more cancers than we do.”
Hicks and the radiologists at RMI found the software to be particularly helpful not just in finding cancers and reducing the time to read, but also in prioritizing caseloads.
“If I am behind on mammograms, I can easily sort by which ones need to be prioritized. We can be much more efficient in sorting cases and getting things done. Speed is important and this technology really does speed our reading time up,” he added.
Hicks also found that ProFound AI improved radiologist performance as a whole across all of the radiologists in his practice.
“The variability in which people read mammograms is real,” said Hicks. “As a large radiology practice reading 31,000 mammograms per year, we don’t want outliers when it comes to our radiologist performance. ProFound AI acts as a friend in the room for radiologists and actually helps them to learn and improve over time.”
The Bottom Line
As the owner and CEO of RMI, Hicks is not only concerned about the health of his patients, he is also concerned about the welfare of the business. Although adopting DBT offered better image quality and more information than ever before, the time it took to read cases was starting to affect the company’s bottom line.
“Although DBT offered improved image quality, we found it required a steep learning curve and the increased workload resulted in a case backlog that required additional staffing to combat,” Hicks mentioned. “For example, a radiologist reviewing 100 cases per day with 2-D would typically review 400 images per day, whereas a radiologist reading 100 cases per day with DBT would be required to read almost 30,000 images per day.” (See Table 1.)
“ProFound AI improved our reading efficiency and eliminated the need to hire more staff,” he added. “The cost of ProFound AI pays for itself based on improved productivity alone.”
For more information: www.icadmed.com
Reference
1. Conant, E. et al. (2019). Improving Accuracy and Efficiency with Concurrent Use of Artificial Intelligence for Digital Breast Tomosynthesis. Radiology: Artificial Intelligence. 1 (4). Accessed via https://pubs.rsna.org/doi/10.1148/ryai.2019180096


 March 06, 2026
March 06, 2026