October 31, 2017 — Some women, because of genetic predisposition, personal or family history, have a higher than average lifetime risk of developing breast cancer. For those women, earlier magnetic resonance imaging (MRI) is recommended for cancer screening.
But according to new findings presented at the American College of Surgeons Clinical Congress 2017, Oct. 22-26 in San Diego, the vast majority of women in one health system who are at higher risk of breast cancer choose not to get breast MRI screenings, even when the service was available to them at no cost.
"The military health system is an equal-access, no-cost system. This system allows us to study how well we are doing in terms of truly adhering to the current recommended guidelines for screening of breast cancer," said lead study author Vance Sohn, M.D., a surgical oncologist at Madigan Army Medical Center, Tacoma, Wash.
For the study, investigators from Madigan Army Medical Center analyzed data on 1,057 women who had a 20 percent or greater lifetime risk of developing breast cancer. The screenings were offered based on their high-risk status, and not because of mammography results. Between 2015 and 2016, these women were offered MRI screenings. The aim of this analysis was to assess whether these higher risk women actually got the imaging test. Overall, the study showed that only 23 percent (247 women) underwent MRI screening.
Further, when results were expressed in quartiles, researchers found that just 15 percent of women with a 20 to 24 percent lifetime risk of breast cancer had an MRI; 24 percent of those with a 25 to 29 percent risk got the imaging test; 36 percent of women with a 30 to 39 percent risk sought an MRI; and only half of the women with more than a 40 percent lifetime risk of developing breast cancer chose to get this recommended screening.
"In the interest of helping more women be screened earlier for breast cancer, we were intrigued about what this preliminary study identified — that 85 percent of women with a 20 to 24 percent lifetime risk still did not pursue high-risk surveillance," Sohn reported. "Ultimately, the question we are really trying to answer is why women at high risk for breast cancer are declining MRI screening. That issue is the next phase of this study."
Sohn and his team plan further research to find out why, on an individual basis, women are declining this cancer check. Is it confusion about the screening tool itself and its safety? Are they afraid of what the test might reveal?
"If we understand the reason behind this circumstance, it will help us better target those who would benefit from this imaging modality so we could provide clear explanations about the test," Sohn said. "The general sense is that patients are just too busy, but discovering the reason will be a very important piece to this puzzle."
Although this was a military health system study, Sohn said he does not think their findings are unique to the military. "In fact, I imagine our compliance rate is even higher than most. Within the civilian healthcare system, there are fiscal implications such as the cost of the MRI and future health insurance implications, that we are controlling for," he said.
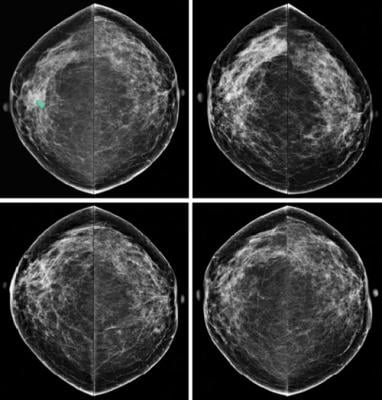
In general, when it comes to breast cancer screening more is not necessarily better. In the past, the misuse of screening MRIs has created much anxiety in women, leading clinicians to perform further testing for tiny spots that turn out to be benign. To target patients for appropriate testing, clinicians and patients alike need a full understanding of the pros and cons of MRI screening. Clinicians then can develop personalized screening plans.
What the study does highlight is that the appropriate application of this imaging technology is very important, Sohn said.
"So maybe the 20 to 24 percent lifetime risk isn't really appropriate, maybe it should be even higher than what the organizations are recommending. In other words, what is the appropriate cutoff?
Ultimately, that is really what we are trying to decipher," he concluded.
For more information: www.facs.org


 February 06, 2026
February 06, 2026 









