Getty Images
September 1, 2020 — Diagnosing respiratory illness associated with vaping has always been challenging. Adding the spread of COVID-19 and the many similarities in symptoms makes it even more difficult.
There are no tests for e-cigarette, or vaping, product use-associated lung injury, known by the acronym, EVALI, which has sickened 2,800 people and killed 68 Americans as of February. Physicians can only diagnose EVALI by first ruling out other conditions that it’s not, a task that is further complicated by patients not always disclosing that they vape.
While cases of EVALI have dropped since their peak in September 2019, they are now once again climbing, and the COVID-19 pandemic has made diagnosing the condition even more difficult since both illnesses share symptoms.
“EVALI is still happening, and on the rise again as people use vaping to cope with pandemic stress,” said Denitza Blagev, M.D., a pulmonary medicine physician at Intermountain Healthcare. “It’s important for clinicians to keep EVALI in mind as they are considering COVID. EVALI has a different prognosis and therapies that we can use to treat these patients, as long as we can diagnose them.”
This comes on the heels of a new study by researchers at Stanford University this week that found vaping is linked to a substantially increased risk of COVID-19 among teenagers and young adults, according to a new study led by researchers at the Stanford University School of Medicine.
The study, published online Aug. 11 in the Journal of Adolescent Health, is the first to examine connections between youth vaping and COVID-19 using U.S. population-based data collected during the pandemic.
The study found that among young people who were tested for the virus that causes COVID-19, the research found that those who vaped were five to seven times more likely to be infected than those who did not use e-cigarettes.
“Patients who contract EVALI or COVID and suffer the same levels of respiratory failure tend to have divergent outcomes,” said Sean J. Callahan, M.D., assistant professor of pulmonary and critical care medicine at University of Utah Health. “Patients with EVALI require a high level of oxygen, but still tend to do well, whereas someone with COVID needing the same level of oxygen support may not do as well. Getting the diagnosis right is vital.”
In a new study published in the journal CHEST, researchers from Intermountain Healthcare and University of Utah Health looked at all patients diagnosed with EVALI at their institutions since March 2020, when COVID tests were readily available in Utah. They found a total of 12 people, who were diagnosed with EVALI who had a negative flu test and at least one negative COVID-19 test between March 1 and May 15. They found that both illnesses showed similar symptoms: respiratory failure, gastrointestinal distress and/or ground glass opacities in the lungs.
Making accurate EVALI diagnoses even more difficult are patients who didn’t admit that they vaped, even after being asked repeatedly. In some cases, clinicians didn’t know someone’s true vaping history until well into the hospital course.
“This is a situation in which you’ve got to ask the patient repeatedly and hope they eventually volunteer the truth,” said Callahan. “It’s crucial for diagnosis.”
Researchers did, however, find two important differences that can help differentiate between EVALI and COVID-19.
First, COVID-19 often leads to normal or low white blood cell counts, while 11 of the 12 EVALI patients showed an increased white blood cell count. Second, patients with severe EVALI tended to be young, with a mean age of 30.8 years old. While COVID-19 can severely affect younger adults, it’s relatively uncommon.
While treatments for COVID-19 are being evaluated, EVALI patients typically respond well to proven to established treatments, such as to corticosteroids. Blagev and Callahan said this is why physicians should consider EVALI when evaluating patients who test negative for COVID-19.
“The risk of missing other diseases that can present with similar and non-specific symptoms, such as a cough or shortness of breath, remains during this time,” said Blagev.
She said while it’s more challenging to diagnose in the time of COVID, EVALI remains an important diagnosis to consider in patients, particularly after an initial negative COVID test.
“First, and foremost, it’s important to keep EVALI in mind because that diagnosis has different treatment and prognosis than COVID. Equally important during a pandemic is ruling out COVID before making the diagnosis of EVALI,” she added.
For more information: www.intermountainhealthcare.org
Related Vaping Content:
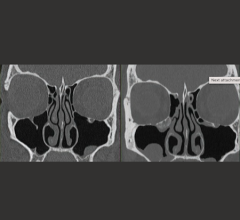
Lung Injuries from Vaping Have Characteristic Patterns on CT
Best Practice Treatment Guidelines Help Doctors Identify, Treat Vaping-associated Lung Injuries
COVID-19: Pediatric Findings in New Review of Lung Disorders
Abnormal Imaging Findings Key to EVALI Diagnosis in Vapers
Radiology: Cardiothoracic Imaging Publishes Special Report on Vaping


 February 16, 2026
February 16, 2026