January 18, 2017 — Researchers from Elizabeth Wende Breast Care (EWBC) have demonstrated that automated volumetric breast density has a strong linear relationship to mammographic sensitivity. These results could improve screening outcomes by defining more appropriate thresholds for identifying the women who may benefit from adjunct screening.
Results of the study, “Using volumetric breast density to quantify the potential masking risk of mammographic density,” published in the American Journal of Roentgenology (AJR), showed that volumetric breast density reflects the sensitivity of mammography – which is tied to the masking risk of breast density – more precisely than visually-assigned Breast Imaging-Reporting and Data System (BI-RADS) density assessment categories. The results also demonstrated that volumetric breast density was associated with the risk of being diagnosed with an interval cancer.
“Breast density has repeatedly been shown to be a significant factor in masking risk and the reduced sensitivity of mammography. The visual assessment of density is subjective and may not provide reproducible results. This becomes more important as we design screening protocols and make decisions about adjunctive imaging for women with dense breasts,” said Stamatia Destounis, M.D., EWBC, clinical professor, University of Rochester School of Medicine & Dentistry. “Our results demonstrated that automated volumetric data shows a strong linear correlation to mammographic sensitivity and can predict the risk of interval cancers. This could be used to define more appropriate cut-offs, or thresholds, for women who may benefit from adjunct screening.”
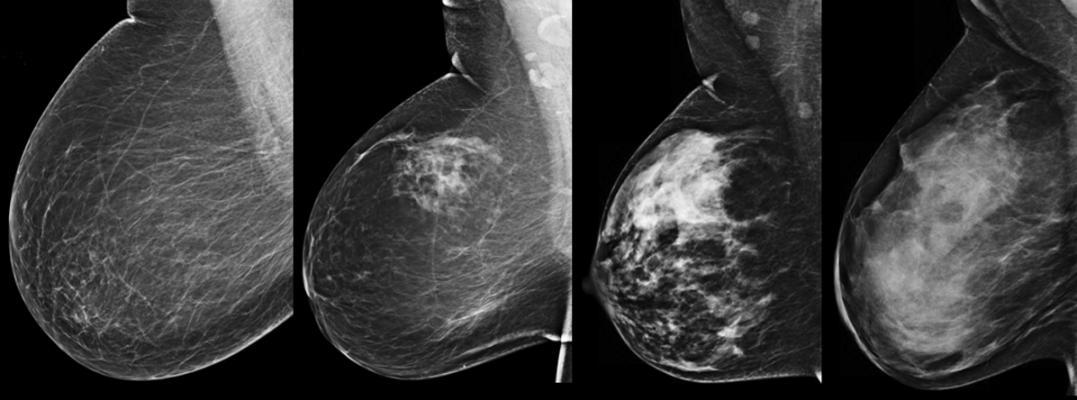
The study included 771 breast cancers (652 screen-detected and 119 interval cancers) diagnosed at EWBC between 2009 and 2012. Breast density was assessed using both the ACR BI-RADS 4th Edition and VolparaDensity, a commercially available software tool. VolparaDensity automatically generates an objective measurement of volumetric breast density as both a continuous percentage and as Volpara Density Grades (VDG), which correspond to the BI-RADS density categories. Mammographic sensitivity was compared between the density assessment methods and within each VDG category, by dividing each category into “high” and “low” using the volumetric breast density mid-point of each VDG.
Overall, mammographic sensitivity in the study cohort was 85 percent. Across visual BI-RADS categories, fatty replaced to extremely dense, mammographic sensitivity was 82 percent, 90 percent, 84 percent and 66 percent, respectively. Using VolparaDensity categories, mammographic sensitivity was 95 percent, 89 percent, 83 percent and 65 percent across VDG categories 1-4, respectively. The linear relationship between mammographic sensitivity and breast density was stronger when using the automated VDG categories than when using visually-assigned BI-RADS categories.
In addition, the results also demonstrated that there was a wide range in mammographic sensitivity within density categories. This suggests that important information relating to masking risk may be missed using BI-RADS categories. While sensitivity was similar for women at the lower and upper end of the VDG1 and VDG2 categories, sensitivity decreased significantly between low and high VDG3 women (i.e. decreased from 86 percent to 77 percent) and low and high VDG4 women (i.e. decreased from 72 percent to 58 percent). Additionally, women with extremely dense breasts (VDG4) category were 4.7 times as likely as women with fatty breasts (VDG1 or VDG2) breasts to have a diagnosis of interval cancer versus screen-detected cancer.
The finer break-down of the automated density categories based on the continuous volumetric density score can thus allow an even more precise assessment of masking risk — something that is not achievable with the visually-assessed BI-RADS categories. According to Destounis, these results suggest there may be women with dense breasts who still have an acceptable level of sensitivity and may benefit less from adjunct screening and reinforces the need for effective communication and education of mammographic sensitivity to referring physicians and patients. Rather than the current approach of presenting a density score to the woman, these findings indicate that an alternative method might be to present a woman with the average sensitivity for women with the same breast density, allowing her to make a more educated decision regarding adjunct screening.
“For women with dense breasts there is a large range in sensitivity that is not being captured using the visual BI-RADS system which could impact the selection of women who would most likely benefit from supplemental imaging. The ability to use automated density measures to capture this masking risk and present it in the form of mammographic sensitivity may more accurately support screening protocols that are based on women’s personal breast density and other risk factors,” added Destounis.
For more information: www.ajronline.org
References
Destounis, S., Johnston, L., Highnam, R., Arieno, A., et al. "Using Volumetric Breast Density to Quantify the Potential Masking Risk of Mammographic Density," American Journal of Roentgenology. Published January 2017. DOI:10.2214/AJR.16.16489


 February 18, 2026
February 18, 2026 









