October 30, 2009 - By using positron emission tomography (PET) researchers were to able to identify neuroinflammation, which is marked by activated microglia cells (brain cells that are responsive to injury or infection of brain tissue) in patients with schizophrenia and in animal models with migraines. This information could tell researchers more about why certain neurologic disorders, such as migraine headaches and psychosis in schizophrenic patients, occur and provide insight into how to best treat them, according to two studies published in the November issue of The Journal of Nuclear Medicine.
Although neuroinflammation has been shown to play a major role in many neurodegenerative disorders—such as multiple sclerosis, Parkinson's disease and Alzheimer's disease—only limited data exists about the role of neuroinflammation in schizophrenia and migraines. The two studies in The Journal of Nuclear Medicine are the first to identify neuroinflammation in specific regions of the brain—a development which could be used to effectively evaluate the treatment response to anti-inflammatory drugs and become transformative for diagnosis and care.
"This study shows that molecular imaging can play an important role in better understanding the processes involving psychiatric and other neurological disorders," said Janine Doorduin, M.Sc., a researcher at the University Medical Center Groningen in the Netherlands and lead author of "Neuroinflammation in Schizophrenia-Related Psychosis: A PET Study." Doorduin added: "Without molecular imaging, the only way to look at inflammation in the brain, as well as other molecular processes, would be to use post-mortem brains."
Not much is known about the cause of schizophrenia—a chronic and disabling brain disease characterized by psychotic episodes of delusions and hallucinations. Previously, evidence from post-mortem studies suggested the presence of activated microglia cells in the brain. However, the results of those studies were inconsistent. Using PET imaging to noninvasively image the living brains of schizophrenic patients, researchers in the Netherlands were able to pinpoint the neuroinflammation to an exact location in the brain, called the hippocampus. Now, researchers can target the hippocampus for further study and evaluate therapeutic treatments that could improve the quality of life for patients living with schizophrenia.
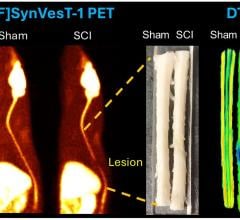
Likewise, PET imaging is also useful for identifying neuroinflammation associated with migraines. In the article, "11C-PK11195 PET for the In Vivo Evaluation of Neuroinflammation in the Rat Brain After Cortical Spreading Depression," researchers in Japan were the first to noninvasively visualize neuroinflammation in an animal model of migraine using a PET technique. Neuroinflammation is thought to be a key factor in the generation of pain sensation in migraine headaches. Observations from the study suggest that an inflammatory process may be involved in the pathologic state of migraines and that PET is a useful tool for evaluating the neurogenic inflammation in vivo.
"For physicians and patients, it is important to develop an objective method for the diagnosis of migraines and monitor therapeutic efficacy," said Yi-Long Cui, Ph.D., a researcher at the RIKEN Center for Molecular Imaging Science in Kobe, Japan, and lead author of the study. "The present study will bring about these possibilities to us since the PET probe used in the paper has already been applied to patients in other diseases."
Co-authors of "11C-PK11195 PET for the In Vivo Evaluation of Neuroinflammation in the Rat Brain After Cortical Spreading Depression" include Yilong Cui, Yosky Kataoka, Yasuhisa Tamura, Cellular Function Imaging, RIKEN Center for Molecular Imaging Science, Kobe, Hyogo, Japan; Tadayuki Takashima, Yasuhiro Wada, Yasuyoshi Watanabe, Molecular Probe Dynamics, RIKEN Center for Molecular Imaging Science, Kobe, Hyogo, Japan; Misato Takashima-Hirano, Hisashi Doi, Molecular Imaging Labeling Chemistry, RIKEN Center for Molecular Imaging Science, Kobe, Hyogo, Japan; and Miho Shukuri, Hirotaka Onoe, Functional Probe Research Laboratories, RIKEN Center for Molecular Imaging Science, Kobe, Hyogo, Japan.
Co-authors of "Neuroinflammation in Schizophrenia-Related Psychosis: A PET Study" include: Janine Doorduin, Erik F.J. de Vries, Antoon T.M. Willemsen, Rudi A. Dierckx, Hans C. Klein, Department of Nuclear Medicine and Molecular Imaging, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands; Jan Cees de Groot, Department of Radiology, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands; and Hans C. Klein, University Center of Psychiatry, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
For more information: jnm.snmjournals.org


 February 13, 2026
February 13, 2026