September 28, 2012 — New optical imaging technology developed at Tufts University School of Engineering could give doctors new ways to both identify breast cancer and monitor individual patients' response to initial treatment of the disease. A five-year clinical study of the procedure, funded by a $3.5 million grant from the National Institutes of Health, is now underway at Tufts Medical Center in Boston.
The noninvasive technology uses near infrared (NIR) light to scan breast tissue, then applies an algorithm to interpret that information. Differences in light absorption allow identification of water, fats, and oxygen-rich and oxygen-poor tissue, the primary structures in breast tissue.
"The consensus is that X-ray mammography is very good at detecting lesions, but it's not as good at determining which suspicious lesions are really cancer," said Sergio Fantini, Ph.D., professor of biomedical engineering, who is leading the research effort. The Tufts NIR technique could complement standard mammography, particularly for women younger than 40 who may have dense breast tissue that tends to obscure detail in X-rays.
Because it does not use ionizing radiation, the NIR technique can be applied multiple times over a short period without risk of radiation exposure, Fantini notes. Another advantage of the technology is that, unlike other breast imaging methods, it can obtain functional real-time images of metabolic changes, such as levels of hemoglobin concentration and oxygenation.
"It's been reported that patients who respond to breast cancer chemotherapy show a decrease in hemoglobin and water concentration and an increase in lipid concentration at the cancer site," explained Fantini. "This suggests that NIR imaging can be valuable not only in diagnosing breast cancer, but in monitoring individual response to therapies without requiring repeated X-rays. For example, it could help determine if a patient is responding to neoadjuvant chemotherapy administered to shrink a tumor before surgery."
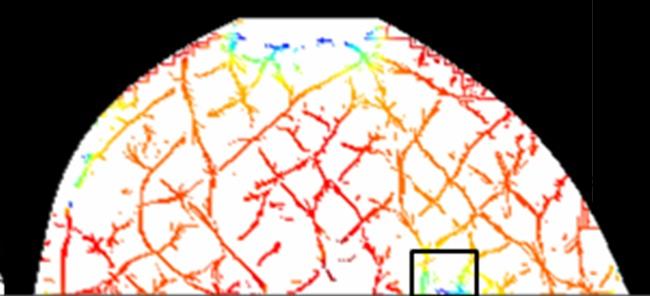
Optical mammography is also more comfortable than traditional mammograms. The patient's breasts are only lightly compressed between two horizontal glass panels and then illuminated by NIR light. A specialized software program displays real-time images of the breast as the optical system scans back and forth. A light detector within the system displays the intensity of the NIR beam as it is transmitted through the breast.
By using an algorithm based on the optical information, the technology generates breast images using the intensity of the transmitted light. The images are displayed automatically and can be read soon after the procedure, as is the case with X-ray mammograms. The technology can be packaged into compact, portable and handheld devices.
Clinical Testing
In collaboration with Roger Graham, M.D., director of Tufts Medical Center's Breast Health Center, and Marc Homer, M.D., chief of mammography at Tufts Medical Center, Fantini and his team conducted "proof of concept" tests to see if their procedure could corroborate information gathered with X-rays on two patients who each had suspicious lesions in one of their breasts.
The optical imaging was successful in enabling the team to identify cancerous tissue. "The test results were compatible with what we found in the X-ray mammography," Graham explained. "It was also painless for the patients and eliminated radiation exposure."
The team also includes Eric Miller, Ph.D., professor and chair of electrical and computer engineering, and Misha Kilmer, Ph.D., professor of mathematics within the School of Arts and Sciences.
The NIH-funded study will investigate healthy women, women with breast cancer and women with benign breast lesions in an effort to examine the effectiveness of optical mammography in detecting breast cancer and distinguishing between malignant and benign tumors. The study will also look at breast cancer patients who are undergoing chemotherapy in order to characterize the power of optical mammography to determine patient response at the beginning of therapeutic treatment.
For more information: http://ase.tufts.edu/biomedical/research/fantini/publications/opticalMa…


 February 17, 2026
February 17, 2026 









