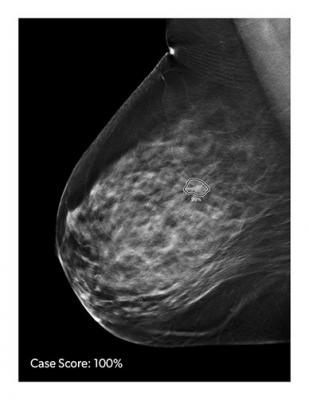
Image courtesy of iCAD
Use of 3-D mammography, an advanced form of breast cancer screening, has risen rapidly in recent years, according to Yale researchers in a new study. But adoption of the technology varies widely, reflecting emerging disparities in care, they said. The study was published in the journal JAMA Internal Medicine.
Three-D mammography is also commonly called digital breast tomosynthesis, or DBT. The technology combines low-dose X-rays with software that creates a 3-D image of the breast. Compared to 2-D mammography, DBT may make it easier for radiologists to detect an abnormality. Yet DBT has not been widely endorsed for routine breast cancer screening. Organizations like the U.S. Preventive Services Task Force and the American Cancer Society, which provide guidance to clinicians about cancer screening, have not made recommendations for or against the routine use of DBT.
To assess the extent of DBT use nationwide, the Yale team examined claims data from private health insurance plans. Their investigation included more than 9 million screening exams performed over three years. They also compared DBT use with privately insured versus Medicare-insured patients.
The researchers found that DBT use rose substantially, from 12.9% to 43.2% of screening exams between 2015 and 2017. The increase was consistent among women who were privately insured and women with Medicare.
"DBT has become very popular overall, although uptake has been uneven. In some areas of the country, it is rarely used while in others, it is the predominant mode of screening," said corresponding author Ilana Richman, M.D., assistant professor in the Section of General Internal Medicine at the Yale School of Medicine.
Richman and her co-authors also observed that adoption of DBT varied greatly by region and demographics. Use of the technology grew more quickly in the Northeast and Northwest but more slowly in the Southeast. DBT was more rapidly adopted in areas with higher incomes, greater education, and larger white populations, they said.
While there is evidence that DBT may boost cancer detection rates and reduce false-positive results, more research is needed to determine the true impact of the technology on breast cancer mortality, said the researchers.
"Although there is a lot of interest in this new technology, we don't know much about how it will affect the long-term health of women," Richman noted. "There are ongoing studies designed to answer these questions, and we hope to have clearer answers in the next few years."
The authors predict that, given these findings, DBT will replace 2-D mammography as the standard of care. "These findings highlight how quickly changes in medical practice -- the rate that doctors adopt these new tests -- can eclipse our ability to evaluate whether they are helping patients to live longer and healthier lives," said senior author and professor of medicine Cary Gross, M.D.
The other Yale authors are Jessica Hoag, Xiao Xu, Howard Forman, Regina Hooley, and Susan Busch.
The Yale researchers accessed the deidentified data through Yale University's participation in the Blue Cross Blue Shield Alliance for Health Research (BCBS Alliance), which engages leading U.S. healthcare researchers in collaborative efforts to improve the health of Americans. Funding for this work was provided by a National Institutes of Health/National Center for Advancing Translational Sciences grant (KL2 TR001862) and by the American Cancer Society. Richman received grants from NIH/NCATS and fees from the Centers for Medicare and Medicaid. Additional disclosures are reported in JAMA Internal Medicine.


 February 18, 2026
February 18, 2026 









