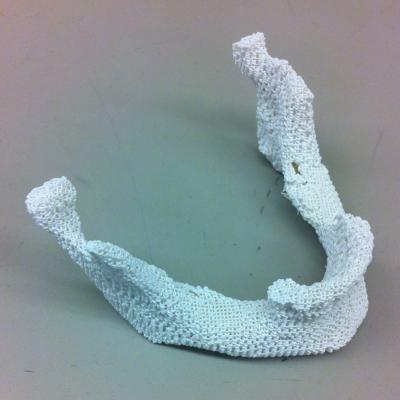
A sample 3-D printed scaffold that matches the lower jaw of a female patient. Image courtesy of Johns Hopkins Medicine.
May 24, 2016 — To make a good framework for filling in missing bone, mix at least 30 percent pulverized natural bone with some special man-made plastic and create the needed shape with a 3-D printer. That’s the recipe for success reported by researchers at The Johns Hopkins University in a paper published online in ACS Biomaterials Science & Engineering.
Each year, the Johns Hopkins scientists say, birth defects, trauma or surgery leave an estimated 200,000 people in need of replacement bones in the head or face. Historically, the best treatment required surgeons to remove part of a patient’s fibula (a leg bone that doesn’t bear much weight), cut it into the general shape needed and implant it in the right location. But, according to Warren Grayson, Ph.D., associate professor of biomedical engineering at the Johns Hopkins University School of Medicine and the report’s senior author, the procedure not only creates leg trauma but also falls short because the relatively straight fibula can’t be shaped to fit the subtle curves of the face very well.
That has led investigators to 3-D printing, or so-called additive manufacturing, which creates three-dimensional objects from a digital computer file by piling on successive, ultrathin layers of materials. The process excels at making extremely precise structures — including anatomically accurate ones — from plastic, but “cells placed on plastic scaffolds need some instructional cues to become bone cells,” said Grayson. “The ideal scaffold is another piece of bone, but natural bones can’t usually be reshaped very precisely.”
In their experiments, Grayson and his team set out to make a composite material that would combine the strength and printability of plastic with the biological “information” contained in natural bone.
They began with polycaprolactone, or PCL, a biodegradable polyester used in making polyurethane that has been approved by the U.S. Food and Drug Administration (FDA) for other clinical uses. “PCL melts at 80 to 100 degrees Celsius (176 to 212 Fahrenheit) — a lot lower than most plastics — so it’s a good one to mix with biological materials that can be damaged at higher temperatures,” said Ethan Nyberg, a graduate student on Grayson’s team.
PCL is also quite strong, but the team knew from previous studies that it doesn’t support the formation of new bone well. So they mixed it with increasing amounts of “bone powder,” made by pulverizing the porous bone inside cow knees after stripping it of cells.
“Bone powder contains structural proteins native to the body plus pro-bone growth factors that help immature stem cells mature into bone cells,” said Grayson. “It also adds roughness to the PCL, which helps the cells grip and reinforces the message of the growth factors.”
The first test for the composite materials was printability, Grayson said. Five, 30 and 70 percent bone powder blends performed well, but 85 percent bone powder had too little PCL “glue” to maintain clear lattice shapes and was dropped from future experiments. “It was like a chocolate chip cookie with too many chocolate chips,” said Nyberg.
To find out whether the scaffolds encourage bone formation, the researchers added human fat-derived stem cells taken during a liposuction procedure to scaffolds immersed in a nutritional broth lacking pro-bone ingredients.
After three weeks, cells grown on 70 percent bone powder scaffolds showed gene activity hundreds of times higher in three genes indicative of bone formation, compared to cells grown on pure PCL scaffolds. Cells on 30 percent bone powder scaffolds showed large but less impressive increases in the same genes.
After the scientists added the key ingredient, beta-glycerophosphate, to the cells’ broth to enable their enzymes to deposit calcium, the primary mineral in bone, the cells on 30 percent scaffolds produced about 30 percent more calcium per cell, while those on 70 percent scaffolds produced more than twice as much calcium per cell, compared to those on pure PCL scaffolds.
Finally, the team tested their scaffolds in mice with relatively large holes in their skull bones made experimentally. Without intervention, the bone wounds were too large to heal. Mice that got scaffold implants laden with stem cells had new bone growth within the hole over the 12 weeks of the experiment. And computed tomography (CT) scans showed that at least 50 percent more bone grew in scaffolds containing 30 or 70 percent bone powder, compared to those with pure PCL.
“In the broth experiments, the 70 percent scaffold encouraged bone formation much better than the 30 percent scaffold,” said Grayson, “but the 30 percent scaffold is stronger. Since there wasn’t a difference between the two scaffolds in healing the mouse skulls, we are investigating further to figure out which blend is best overall.”
Although the use of “decellularized” cow bone has been FDA-approved for clinical use, in future studies, the researchers say, they hope to test bone powder made from human bone since it is more widely used clinically. They also want to experiment with the designs of the scaffolds’ interior to make it less geometric and more natural. And they plan to test additives that encourage new blood vessels to infiltrate the scaffolds, which will be necessary for thicker bone implants to survive.
Other authors of the report include Ben Hung, Bilal Naved, Miguel Dias, Christina Holmes, Jennifer Elisseeff and Amir Dorafshar of the Johns Hopkins University School of Medicine.
This work was supported by the National Institute of Dental and Craniofacial Research (F31 DE024922), the Russell Military Scholar Award, the Department of Defense, the Maryland Stem Cell Research Fund and the American Maxillofacial Surgery Society Research Grant Award.
For more information: www.pubs.acs.org/journal.abseba

 April 18, 2025
April 18, 2025 









