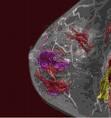
December 15, 2008 - Magnetic resonance imaging (MRI) alternated with mammography at six-month intervals can detect breast cancers not identified by mammography alone, according to a study by researchers at The University of Texas M. D. Anderson Cancer Center. MRI is known to be more sensitive in detecting breast cancers than mammography, with a 71 - 100 percent accuracy compared to a 16 - 40 percent accuracy for mammography. As a result, annual breast cancer screening for high-risk women now typically includes MRI along with mammography and a clinical breast exam. "In the high-risk population, the recent standard of practice is to perform mammography and MRI every year," said Huong Le-Petross, M.D., assistant professor of diagnostic radiology at M. D. Anderson and the study's first author. "What we started to do at M. D. Anderson was to see if we could do mammography and then six months later do a breast MRI exam, followed six months later with a mammogram exam, and then six months after that with a breast MRI. That way the women would receive an imaging modality screening every six months." In the pilot study, presented at a poster session on Dec. 13, the researchers performed a retrospective chart review of 334 women who had participated in a high-risk breast cancer-screening program at M. D. Anderson from Jan. 1997 to Dec. 2007. The women had undergone between one and four MRI screening cycles and were considered to be at high risk if they had hereditary breast and ovarian cancer syndrome, a personal history of breast cancer, a biopsy indicating atypia or lobular carcinoma in situ (LCIS), or a 20 percent or higher lifetime risk of developing breast cancer, as estimated by the Gail model. In the all-M. D. Anderson study, 86 of the 334 high-risk women (26 percent) underwent this alternating approach. Among this group, 46 percent completed the first round of MRI screening, 28 percent completed the second round, 13 percent completed the third round, and 4 percent completed the fourth round. The other 248 women underwent prophylactic mastectomy or were started on chemoprevention agents. All study participants were given a clinical breast exam every six months. The median follow-up time was two years, with a range of one to four years). The alternating MRI and mammography screening program detected nine cancers among the 86 women-five invasive ductal carcinomas, three invasive lobular carcinoma, and two ductal carcinomas in situ. Five (55 percent) of these cancers were identified by MRI but not by mammography, three (33 percent) were found by both MRI and mammography, and one (11 percent) cancer, a tumor one millimeter in size, was overlooked by both screening techniques. No cancer was detected by mammography alone. "We found that MRI picked up the majority of cancers, while mammography picked up only three out of the nine," Le-Petross noted. With five of the eight cancers detected by MRI, the mammogram from six months earlier was either normal or suggested benign findings. "The global picture is that MRI can pick up cancers that mammography cannot," Le-Petross said. "This would suggest that in this population it is more beneficial for the patient to have screening MRI so that we can pick up small lesions before a mammogram can detect them." One important unanswered question is whether an alternating MRI and mammography screening program will save lives. "That is going to take a 5- to 10-year follow-up to determine," Le-Petross added. "It is an exciting question because mammography has always been the standard, and now we are challenging that gold standard examination." The authors of the M. D. Anderson study include: Huong Le-Petross, M.D., Gabriel Hortobagyi, M.D., professor and chair of the Department of Breast Medical Oncology; Banu Arun, M.D., associate professor in the Departments of Breast Medical Oncology and Cancer Prevention and the study’s senior author; Deanna Atchley, Department of Breast Medical Oncology; and Gary Whitman, M.D., professor in the Department of Radiology. For more information: www.mdanderson.org


 February 18, 2026
February 18, 2026 









