February 5, 2019 – The American Society of Echocardiography (ASE) released a new document that provides a comprehensive review of the optimal application of transesophageal echocardiography (TEE) for patients with congenital heart disease (CHD).
Congenital heart disease is the most common form of birth defect worldwide. In the United States alone, over 40,000 children are born annually with CHD and the number of children and adults living with CHD is estimated at 2 to 3 million. Transthoracic echocardiography (TTE) has always been an essential non-invasive diagnostic tool for pediatric cardiologists, but recent advances in transesophageal echocardiography (TEE) technology have led to its increasing importance in the care of both children and adults with CHD.
The document, Guidelines for Performing a Comprehensive Transesophageal Echocardiographic Examination in Children and All Patients with Congenital Heart Disease: Recommendations from the American Society of Echocardiography, has been endorsed by over a dozen cardiology societies worldwide and appears in the February issue of the Journal of the American Society of Echocardiography (JASE).
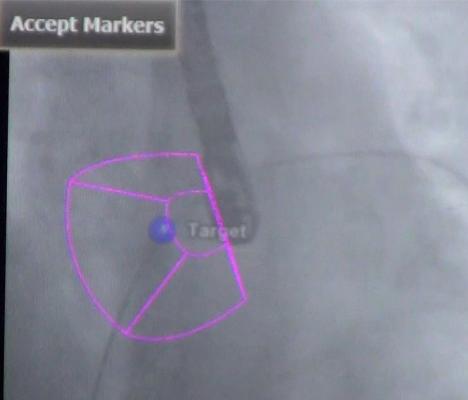
The chair of the writing group, Michael D. Puchalski, M.D., FASE, of the University of Utah, Primary Children’s Hospital in Salt Lake City, commented, “The prior guideline paper for TEE in children and all patients with CHD was published in 2005 and focused primarily on when to do it, how to do it and who should do it. This new paper really expanded on that in a significant way by providing a comprehensive protocol for image acquisition. We recommend numerous views to evaluate a wide variety of congenital heart conditions and have added 3-D echo, which did not exist in 2005. The technologic advancements in the last decade or more have expanded the use of TEE to guide interventions in the catheterization lab and improve operative outcomes from the smallest babies to the oldest adults.”
The document outlines in detail the technical considerations and imaging techniques, as well as the value that TEE can add to the management of specific congenital heart defects. It also details the use of TEE to guide catheter-based interventions, which have become increasingly used in recent years, and addresses the need for specific training and educational pathways specific to the use of TEE in children and CHD patients. The document includes several useful tables, including one that summarizes and illustrates the 28 suggested views for a comprehensive TEE exam in CHD patients.
In conjunction with the publication of the guideline document, Puchalski will conduct a live webinar, including a question and answer section, on March 19 at 10:00 a.m. Eastern Time. The webinar will be available for free to all ASE members and open to all other clinicians for just $25. Registration is open online. This webinar, and all ASE-hosted guideline webinars, are available on ASEUniversity.org to facilitate education for those who cannot attend the live webcast.
This document and all ASE Guideline documents are also available to the medical community at ASEcho.org/Guidelines.
For more information: www.asecho.org


 February 05, 2026
February 05, 2026