May 16, 2014 — An old idea of re-treating lung tumors with radiation is new again, especially with the technological advances seen in radiation oncology over the last decade. The Comprehensive Cancer Center of Wake Forest Baptist Medical Center is one of only a handful of cancer centers that is attempting to give lung cancer patients out of treatment options a chance to keep the cancer at bay. For these patients, hope lies in a second course of treatment – repeat radiation. Two complementary papers published back-to-back recently in the journal Radiotherapy and Oncology and the Journal of Thoracic Oncology outline the treatment success at Wake Forest Baptist.
“One of the toughest challenges of lung cancer is what to do for patients when the cancer comes back in an area that’s been treated previously with radiation treatment,” said James J. Urbanic, M.D., lead author of the studies and a radiation oncologist at Wake Forest Baptist. “With some of the technological advances in radiation treatments that have occurred in the last five to 10 years, we’re beginning to re-look at the issue and ask – can we target the radiation precisely enough and with a high enough dose to knock the cancer back?”
Urbanic said the overall findings of the study suggest that there are some patients with recurrent lung cancers who can be treated with another definitive course of radiation therapy and still have a chance at a cure. “At many cancer treatment centers, these patients only get chemotherapy and have no chance at definitive treatment. The goal of treatment is solely to prevent or delay symptoms from developing, and they are seen as incurable,” he said. “But with re-irradiation, our study shows that maybe we can give a curative intent treatment that we couldn’t do in the past. It’s a layer of hope for some patients that they never had before.”
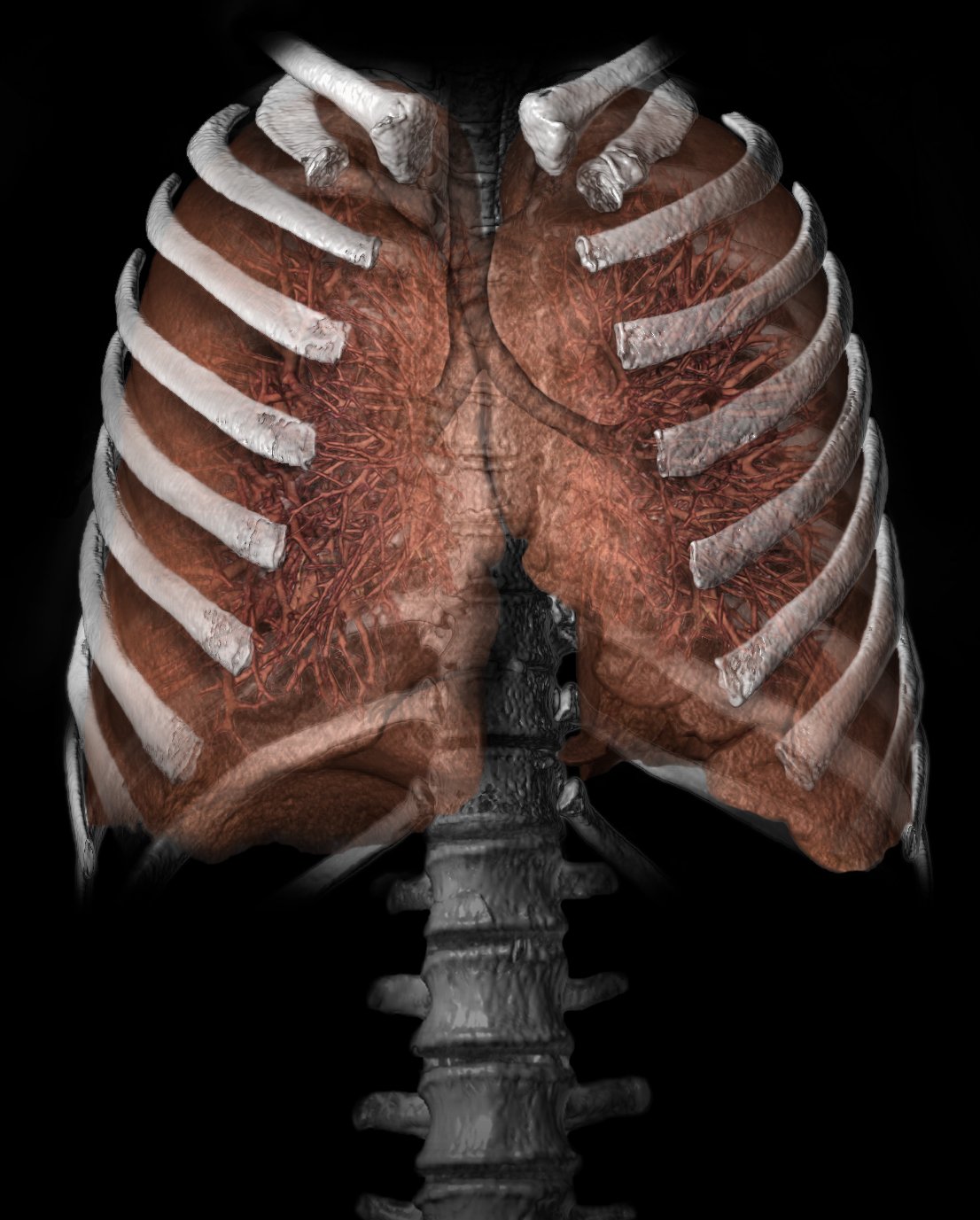
For this study, the researchers looked back at 11 years of clinical data. Eighty-six patients were identified as receiving at least two courses of thoracic radiotherapy. Of that number, 33 were treated with repeat thoracic radiotherapy using stereotactic body radiation therapy (SBRT) or accelerated hypofractionated radiotherapy (AHRT) as a component of their treatment. The median age was 66 and the majority of patients (88 percent) were treated for primary lung cancer. Average tumor size at retreatment was 2.5 cm. Prior lung resections had been completed in 24 percent of patients.
Urbanic said the typical patient is an older man or woman who was treated with either chemotherapy and radiation or radiation alone for a lung cancer that couldn’t be surgically removed. They’ve returned for a checkup and feel well, but a CT (computed tomography) scan shows that the cancer has returned in the area previously treated. If the cancer is just in one spot, the patients get retreated with 10 radiation treatments done with the SBRT technique, which is tightly targeted to just the tumor and minimizes the dose to the surrounding normal tissue.
“Wake Forest Baptist has been developing expertise in doing this,” Urbanic said. “We’re finding that there are patients who are alive years later. We have seen relatively modest toxicity and a good ability to try and control the disease – upwards of 70 percent of the time.”
But there is a higher risk of injury involved when someone is radiated a second time, which is why other cancer treatment center programs might be reluctant to adopt the practice, he said.
“This is a fairly niche effort in lung cancer care, and we’d like to see a national level clinical trial at some point,” he said. “The technology has gotten to the point where I think it’s going to allow radiation oncologists to reassess their ability so that maybe they can take risks they weren’t willing to take before. Eventually, this practice will become more widespread.”
Co-authors include Jeremy M. Kilburn, M.D., Jeffrey G. Kuremsky, M.D., A. William Blackstock, M.D., Michael T. Munley, Ph.D., William T. Kearns, M.S., William H. Hinson, Ph.D., James F. Lovato, M.S., Antonius A. Miller, M.D., and William J. Petty, M.D., all of Wake Forest Baptist.
For more information: www.wakehealth.edu


 January 30, 2026
January 30, 2026 









