Robovision BrainMets AI helps detect, quantify and track brain metastases by producing clear and comprehensive reporting — while keeping existing workflows unchanged. Copyright Robovision Healthcare.
Brain metastases are 10 times more common than primary brain tumors, occurring in 10 to 20% of adult patients with cancer.1 The current limit of detection clinically is 2 to 5 mm in diameter, though metastases are more typically detected between 5 mm and 1 cm.2 Yet in their earliest stages, metastases can be 3 mm or smaller, making them challenging to identify on an MRI.
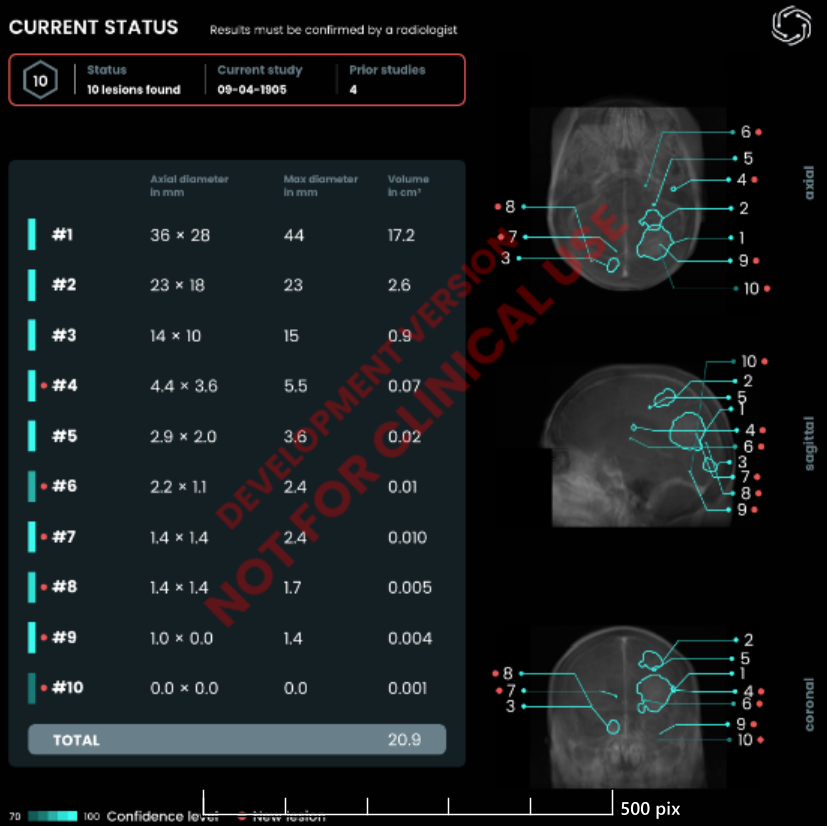
Now, artificial intelligence (AI) models are being studied as potential aids to help radiologists detect and measure these very small lesions with greater accuracy, potentially expanding treatment options and improving survival rates. Researchers at the Netherlands Cancer Institute (NCI) recently evaluated one such solution, BrainMets AI from Robovision Healthcare, against an annotated dataset of more than 1,500 MRI cases from multiple institutions across the United States and Europe.
Results showed that the solution achieved 97.4% lesion-level sensitivity, including 93.3% on sub-3 mm lesions.3 In an external validation set of 311 scans of 260 patients, BrainMets AI identified all true cases of brain metastases, yielding zero false negatives and fewer than 2% false positives.4

“A lot of existing AI solutions were trained on models that can identify primary brain tumors at 6 to 7 mm and above, but miss metastases below that threshold,” says Stephane Willaert, VP Robovision Healthcare, who has spent 25 years in radiology technology, including past leadership roles at Barco. “Clinically, that gap is significant. It could mean a delay of six to 12 months before a diagnosis is confirmed.”
Like Finding a Grain of Sand
What had traditionally made metastases difficult to find early, Willaert says, is that they can blend into the greyscale image of the brain on an MRI.
“An image of the brain is like looking at a bowl of rice,” he says. “Primary tumors are easier to find — like a ping pong ball, marble, or pea sitting in the bowl of rice. But trying to find a small brain metastasis is like trying to find a pinhead or a grain of sand, which is very hard to do.”
To help radiologists find brain metastases sooner, Robovision and the team at NCI built BrainMets AI using a three-part methodology that included a custom model architecture, high-fidelity voxel-level annotations by neuroradiology specialists, and a diverse expertly annotated dataset. “The experts at NCI manually segmented each lesion in detail, adding annotations and performing quality checks,” Willaert says.
A secondary challenge for radiologists, Willaert says, is quantifying the metastases once found. “Right now, the gold standard is axial diameter, but there’s room for improvement, because if you ask five to 10 different radiologists to measure the diameter of a brain metastases, you could get many different measurements,” he says. To overcome this barrier, BrainMets AI provides volumetric measurements of brain metastases automatically, creating more precise assessments and potentially saving time for radiologists.
Potential Workflow Improvements
Radiologists continue to deal with higher rates of burnout, with researchers identifying multiple individual and organizational-directed initiatives to reduce burnout and promote well-being.5 BrainMets AI, Willaert says, can reduce documentation burdens for radiologists by producing a structured report that includes quantification, segmentation, and longitudinal tracking. The report can be shared downstream with oncologists, neuro-oncologists, surgeons, and other providers.
“Feedback we’re hearing from early adopters is the positive impact of the report on Tumor Board meetings,” Willaert says. “These are some of the most expensive meetings in a hospital, with all your highest-paid specialists around the table. Radiologists using BrainMets AI have told us that they’re spending much less time preparing for Tumor Board and are more efficient during the meetings using our report.”
BrainMets AI is currently in clinical validation trials in Europe, with testing underway in the United States. The software is on track to become available in the states next year, pending FDA clearance.
References
- Parker M, Jiang K, Rincon-Torroella J, et al. Epidemiological trends, prognostic factors, and survival outcomes of synchronous brain metastases from 2015 to 2019: a population-based study. Neurooncol Adv. 2023;5(1):vdad015. Published 2023 Mar 5. doi:10.1093/noajnl/vdad015
- Serres S, Soto MS, Hamilton A, et al. Molecular MRI enables early and sensitive detection of brain metastases. Proc Natl Acad Sci U S A. 2012;109(17):6674-6679. doi:10.1073/pnas.1117412109
- Topff L, Petrychenko L, Jain N, et al. A Data-Centric Approach to Deep Learning for Brain Metastasis Analysis at MRI. Radiology. 2025;315(3):e242416. doi:10.1148/radiol.242416
- Topff L, Petrychenko L, Jain N, et al. A Data-Centric Approach to Deep Learning for Brain Metastasis Analysis at MRI. Radiology. 2025;315(3):e242416. doi:10.1148/radiol.242416
- Chetlen AL, Chan TL, Ballard DH, et al. Addressing Burnout in Radiologists. Acad Radiol. 2019;26(4):526-533. doi:10.1016/j.acra.2018.07.001


 February 06, 2026
February 06, 2026 









