October 25, 2013 — Ronald Wheeler, M.D., along with contributing radiologists, authored a clinical study demonstrating the use of
magnetic resonance imaging (MRI) in the diagnosis and treatment of
prostate cancer indicating a greater than 99 percent rate of cure when combined with high-intensity focused ultrasound (HIFU) treatment. The Diagnostic Center for Disease in Sarasota, Fla. studied more than 140 patients and tracked their progress for up to 72 months.
Introduction
More than 250,000 men are diagnosed with prostate cancer yearly through biopsy when the prostate specific antigen reaches 2.5 ng/ml or higher. Referencing the Surveillance, Epidemiology and End Results Program data, there is an expectation that more than 500,000 men will be diagnosed within the next 10 years. To be sure, men and physicians alike are uncertain who should be treated and when they should be treated when a rising Prostate Specific Antigen (PSA) alerts them to a pending problem.
This is a vexing proposition for physicians and patients alike when localized prostate cancer is diagnosed with biopsy and/or a multi-parametric MRI (mp-MRI) scan. This study intends to demonstrate the efficacy of HIFU for all grades of prostate cancer including low grade, intermediate grade and high grade complemented by the use of an mp-MRI scan in all patients.
Methods
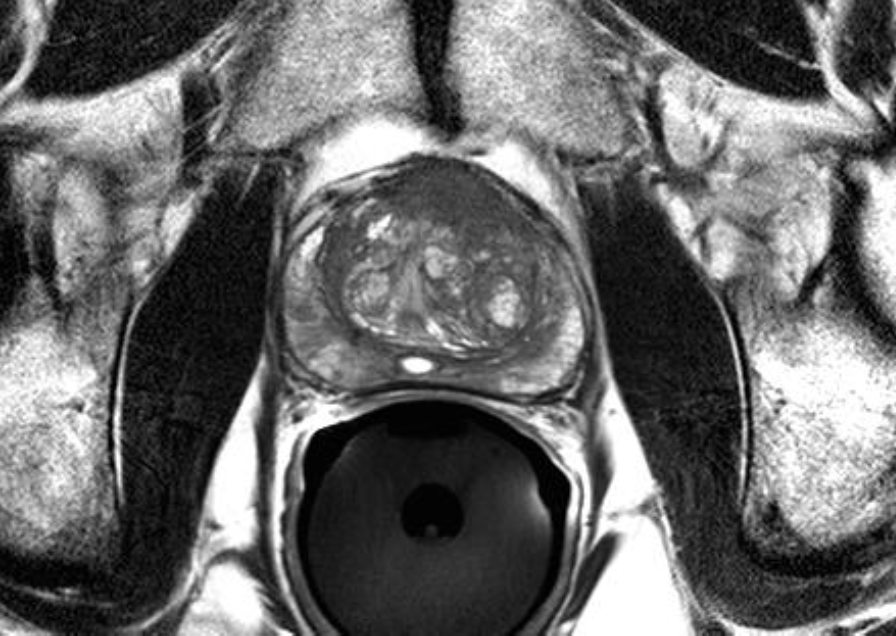
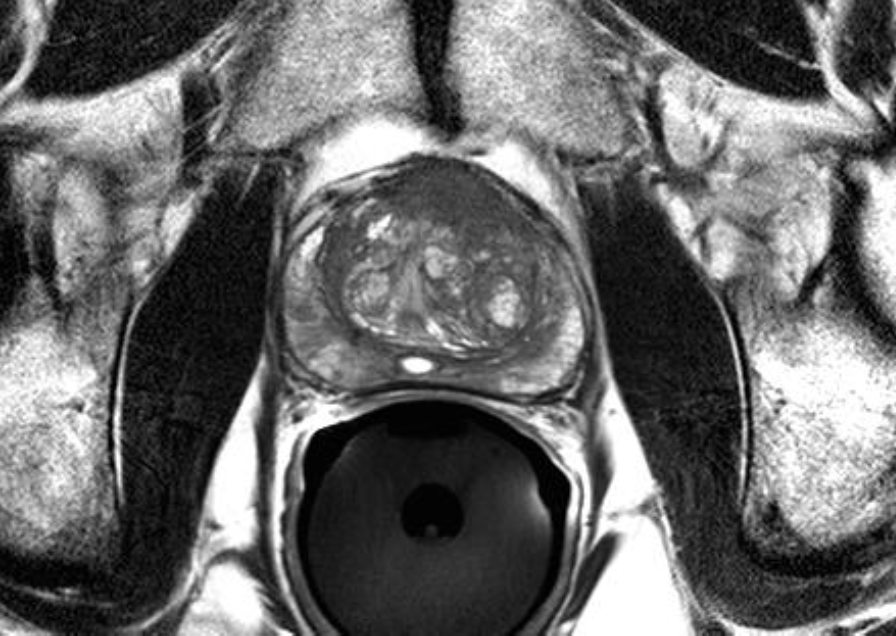
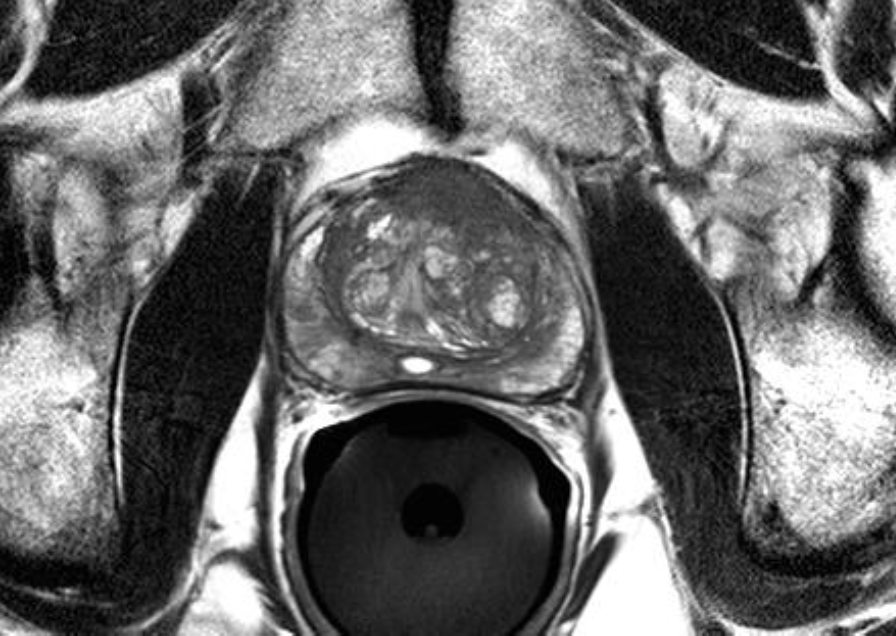
One hundred forty-seven patients diagnosed with prostate cancer from a biopsy or mp-MRI scan independent of a biopsy were treated with a total gland HIFU procedure. All men who had a biopsy confirmation were scanned without prior knowledge of a biopsy and/or results by radiologists who read the scan. Patients had to qualify for this retrospective study by having a PSA value less than or equal to 8.5 ng/ml, a Gleason score less than or equal to 4+4 = 8 while treatment had to be performed within 4 years of the diagnosis. Specifically, 70 patients had biopsy diagnosed prostate cancer indicating Gleason scores of 3+3 = 6, 3+4 = 7, 4+3 = 7 or 4+4 = 8. The total number of patients in each group were 37, 25, 6 and 2 respectively. Additionally, 77 patients had cancer diagnosed with either a 1.5 Tesla Philips MRI (with an endorectal coil), a 3 Tesla GE HDX scan or a Siemens 3.0 Tesla Tim Trio magnet (with or without an endorectal coil). All scans were read by experienced radiologists well-educated in prostate scans relevant to sequences of MRI including T2 weighted images (T2W), dynamic contrast enhancement (DCE) and diffusion weighted images (DWI) without assistance by spectroscopy. All men subsequently underwent treatment by one HIFU treating expert within four years of their diagnosis.
Results
The highest PSA value was recorded for each patient from the biopsy group with a mean PSA value of 5.1 ng/ml with a range of 0.5 to 8.5 ng/ml. The nadir PSA value in the entire biopsy group was 0.28 ng/ml while the breakdown for Gleason scores of 6, 7 and 8 was 0.28 ng/ml, 0.28 ng/ml and 0.15 ng/ml respectively. Likewise, the highest PSA value in the MRI diagnosed group was noted to be 5.5 ng/ml with a range of 0.39 to 8.5 ng/ml. The PSA nadir in the mp-MRI treated group was 0.24 ng/ml.
Success from the HIFU treatment was judged using the Phoenix definition for cure. Ninety-nine percent of the group was cured with the range of follow-up from three months to 72 months. The impressive cure rate is attributed to patient selection, physician expertise and the use of imaging diagnostically and for staging. Equally impressive was a lack of significant side effects with the HIFU procedure. Specifically, urethral narrowing or bladder neck contracture were present in approximately 15-20 percent of patients treated while long-term issues with impotency, incontinence and rectal wall injury was absent.
Conclusion
The outcome data associated with this study should preferentially attract patients diagnosed with prostate cancer to HIFU, thereby considering an outpatient procedure that is indicated as a single treatment. The inclusion of Gleason scores of eight cancers magnifies the added value to a disease grade that heretofore had suffered from poor outcomes with any treatment choice. While encouragement is noted with a very aggressive cancer grade, long-term follow up is needed. Beyond this notation, excitement within the health industry for HIFU as a definitive treatment for men with virtually all grades of prostate cancer promises to take more caustic and invasive commonly used procedures to the alternative category.
Unfortunately, until approval by the Food and Drug Administration (FDA), only a small percentage of the patients diagnosed with prostate cancer will be able to access this level of treatment, as they are dependent on third party payers (insurance companies) to appropriately pay for their procedure. Without FDA approval, doctors will be reluctant to offer the HIFU procedure and ignore training programs while offering inferior treatment options with significant side effects. HIFU requires significant training to achieve excellence in outcome data. Doctors are encouraged to get involved and get educated now if they expect to compete with the best doctors in the world once approved.