Photo courtesy of Elekta.
A prospective study of guideline-based postoperative image-guided intensity modulated radiation therapy (IG-IMRT) in prostate cancer patients found toxicity profiles low and patient-reported quality of life following treatment favorable. Researchers concluded that toxicity and health-related quality of life (HRQOL) should not impact the recommendation of radiation therapy treatment following prostatectomy.
The study, “Phase 2 trial of guideline-based postoperative image guided intensity modulated radiation therapy for prostate cancer: Toxicity, biochemical and patient-reported health-related quality-of-life outcomes,” was published in the September-October 2015 issue of Practical Radiation Oncology (PRO), the American Society for Radiation Oncology’s (ASTRO) journal focused on the clinical practice of radiation oncology.
An Underutilized Therapy?
Post-prostatectomy radiation therapy (RT) has been reported as underutilized, with randomized trials showing the benefit of adjuvant radiation therapy (ART) but approximately only 10 percent of patients receiving the treatment, according to a study published in 2014. One potential reason for underutilization could be concern over side effects or a negative impact on HRQOL. Study authors in the phase 2 trial set out to determine if this reason was accurate using a consensus guideline for defining the clinical target volume, looking at the treatment-related toxicities, HRQOL and biochemical outcomes of patients treated with postoperative IG-IMRT for prostate cancer following prostatectomy.
In the study, 68 men considered for radiation therapy after prostatectomy at the Princess Margaret Cancer Centre/University Health Network, Toronto, were enrolled between August 2007 and October 2008. The median age at diagnosis was 59.8 (range 43.7 – 74.2). Of those, 53 patients (77.9 percent) were treated with salvage RT and 15 (22.1 percent) were treated with ART. Published consensus guidelines were used to delineate the clinical target volume, or prostate bed, with patients receiving a dose of 66 Gy in 33 fractions. The radiation treatment plan prioritized rectal dose constraints over target volume coverage, according to the study authors. IMRT and daily cone beam computed tomographic (CBCT) guidance delivered the treatment. Routine follow-up occurred every three to six months during the first five years. Median follow-up after treatment completion was 5.9 years (range 0.1 – 6.7 years).
Toxicity was graded according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events, while the HRQOL was measured according to the Expanded Prostate Cancer Index Composite (EPIC) questionnaire, which was collected prospectively at baseline, week five (during RT), three months after RT completion and at one-, two-, three- and five-year follow-up visits.
Researchers calculated the cumulative toxicity and biochemical relapse-free rates by the Kaplan-Meier method. Changes in HRQOL were measured using paired student t-tests with multiple testing correction.
According to the study, the main primary planning objectives were met in 97.1 and 98.5 percent of cases (dose received by 99 percent of the planning target volume [PTV] = 54 Gy, and rectal wall maximum dose (1 cc) = 66 Gy, respectively). Secondary PTV coverage objective was volume of PTV receiving at least 95 percent of the prescribed dose = 95 percent, which was met in two-thirds of cases.
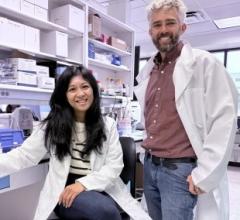
“With modern radiotherapy and the continuous improvements in treatment techniques, the present study rejects the notion that the use of radiation treatment after prostatectomy may have a negative impact in the patient’s quality of life pertaining to sexual, urinary or bowel function,” said study lead and first authors, Cynthia Ménard, M.D., and Alejandro Berlin, M.D., MSc, from the Princess Margaret Cancer Centre/University Health Network, Toronto.
The cumulative five-year incidence of late gastrointestinal Grade 2 was 12.3 percent (95 percent confidence interval [CI], 11.1 percent-13.5 percent) and genitourinary Grade 2 toxicities was 10.6 percent (95 percent CI, 9.5 percent-11.6 percent). No Grade 3 or Grade 4 late toxicities were observed.
Researchers observed transient declines in EPIC gastrointestinal domain summary score (mean 87.66 at three months versus 92.76 at baseline; P = .006) and genitourinary irritative subscale (week five mean score 83.37 versus 89.45 at baseline; P = .007). Complete recovery occurred between three and 12 months after therapy, which remained stable compared with baseline at five-year follow-up.
The sexual HRQOL remained stable at five years, with an improving trend in bother subscale, with the five-year mean score at 58.17 versus 44.81 at baseline. This improvement might be because patients became accustomed to erectile dysfunction over time, Berlin said.
At five years, biochemical relapse-free rate was 72.7 percent (95 percent CI, 61.9 percent-83.5 percent).
Cautionary Notes
The study authors cited weaknesses and cautionary notes from the study, the first being that the study had a relatively small sample size. However, having the patients’ answer the EPIC questionnaire was effective in obtaining results directly impacted by treatment, especially in an area without a great deal of patient-reported information, they said.
“Studies evaluating the results, particularly quality of life, after post-prostatectomy radiotherapy are scarce,” Berlin said. “This is even more relevant with the use of current modern techniques. Despite the small sample size, each patient is his ‘own control,’ as the variations in quality of life are compared to the pre-radiation baseline status, providing strength to the analysis.”
Other weaknesses in the study were the completion rate of the EPIC questionnaire, which declined over time (but the authors cited that, because of the “stability and reproducibility” of results over the follow-up, a clinically meaningful change to results would be small). In addition, they point out that the volume definition of organs at risk may be different at other institutions so “caution should be used in determining the equivalence of other normal tissue dosimetric parameters to be applied for plan evaluation when different contouring techniques are used,” study authors said.
Overall, “results are encouraging and continue to support the use of a well-established treatment for specific indications after prostatectomy, e.g. rising prostate-specific antigen, extraprostatic extension, positive margins, etc., contrasting with the literature reporting that only a small proportion of these actually receive post-operative radiation,” Ménard said.
“Additionally, when consensus definition of target volumes were developed, concerns were raised due to larger volumes compared to historical practice. Therefore, the low toxicity rates observed, particularly rectal toxicity, were positively surprising. This study provides clinical validation and evidence to support the use of current guidelines for post-prostatectomy radiotherapy,” Berlin concluded. itn
Editor’s note: This study’s abstract can be found at www.practicalradonc.org/article/S1879-8500(15)00085-5/abstract.


 February 04, 2026
February 04, 2026