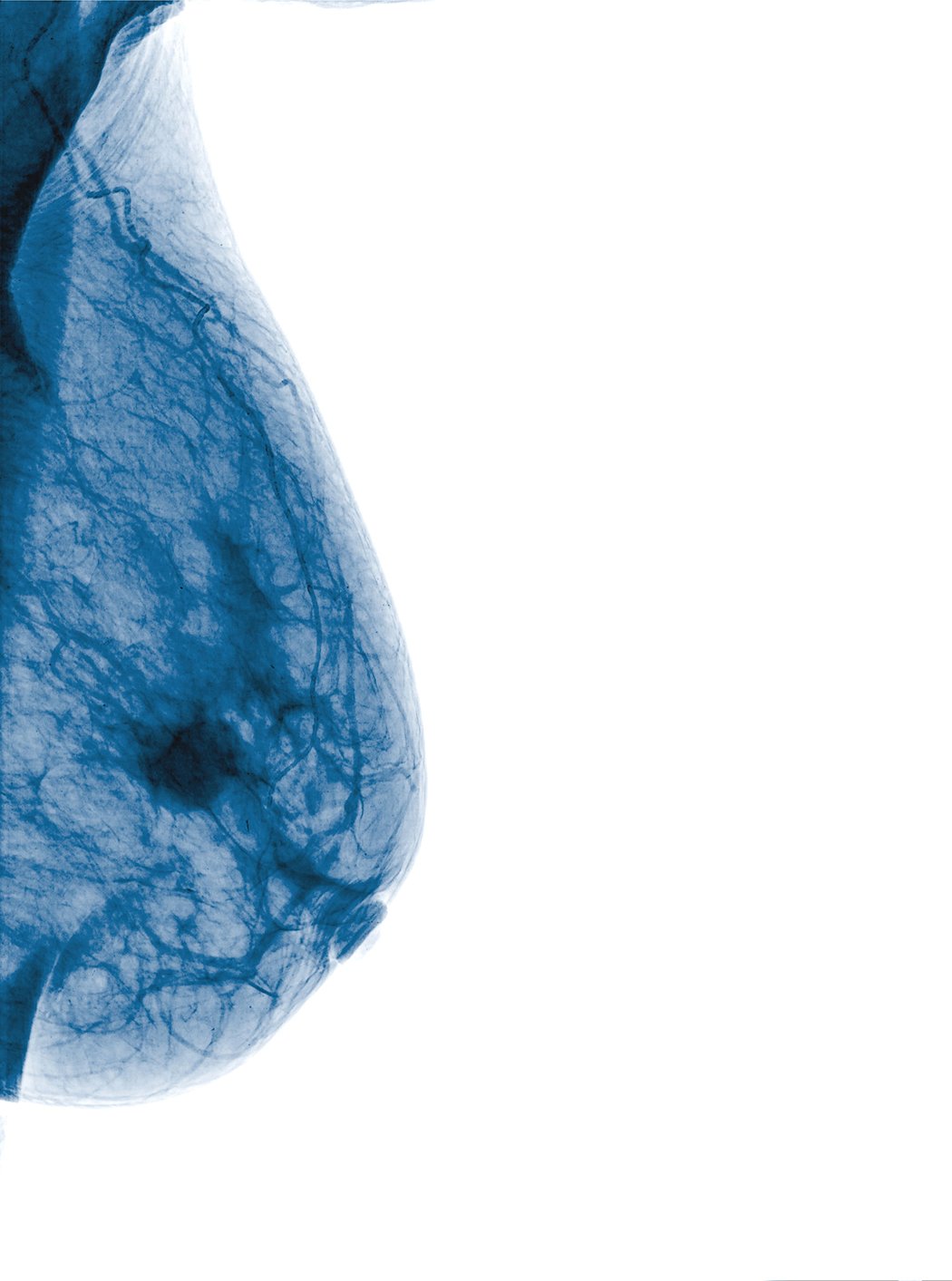
Photo courtesy of Monthian Ritchan-Ad
While mammograms play a vital role in efforts to identify breast cancer, they can present some challenges in women with dense breast tissue. Both dense breast tissue and cancer cells can appear as solid white in mammography, increasing the risk that results might be misinterpreted. Some recent advances in both technology and in communications about breast density have the potential to help clinicians and patients overcome these challenges in the years ahead.
An estimated 40 percent of women over age 40 have dense breasts, which have less fat and more connective, fibrous and glandular tissue compared to lower-density breast tissue. The risk of breast cancer is four to six times greater in women with extremely dense breasts than in women with low breast density,1 reinforcing the need for careful monitoring and effective communication about their risk.
Improving Communication
The issue of communication about dense breast tissue is so important that many states now have laws in place requiring distribution of dense breast notifications (DBNs) directly to women who are found to have dense tissue. These communications are designed to provide basic information and encourage women to discuss the risks associated with dense breast tissue with their doctor. Connecticut was the first state to pass a DBN law in 2009; there are now 31 states that have this requirement in place. While this is an important development for women’s health, some recent research indicates that the quality of these DBN communications can vary widely from state to state.
A recent study published in the Journal of the American College of Radiology suggests that some DBNs may be playing a role in improving patient education and treatment. Following the introduction of DBNs in New Jersey, researchers found that use of screening ultrasounds increased by 651 percent in the 18-month period after the law was enacted. They also found MRIs increased by 59.3 percent, reducing the number of biopsies needed per cancer diagnosis.2 This suggests that DBNs may have helped more women with dense breasts to recognize the need for supplemental screening and to take appropriate action.
The results in Virginia have not been as positive. A survey there shows that many women still do not understand what breast density means and how it can impact the detection of breast cancer despite the fact that DBNs have been mandated since 2012. Among 1,000 women between the ages of 35 and 70, only 25 percent were aware of the relationship between breast density and cancer risk.3 These findings indicate that DBNs may not be helping many women in Virginia develop a better understanding of breast density and the impact it can have on their health.
Variation in the effectiveness of DBNs may be caused in part by the lack of clear guidelines regarding the level of detail they should provide. A recent study published in the Journal of the American Medical Association (JAMA) showed that the language used to explain breast density in DBNs in many states is often overly complex and difficult for most women to understand.4 Also, in some cases DBNs do not provide clear guidance on the next steps women should consider when they have dense breasts, including the potential benefits of additional screening. Some states require that women be informed if their breasts are dense and that additional screening might help to detect breast cancer, while others require only that women be informed about the issue of breast density without providing context regarding the potential implications.
With the variation in tone and level of detail in DBNs, there also is no strong consensus among radiologists regarding their benefits. In a recent study published in the journal Academic Radiology, researchers surveyed 523 members of the New England Roentgen Ray Society. Questions focused on their awareness of breast density legislation and perceived practice changes resulting from density notification. Fully 73 percent of respondents practiced in a state with breast density legislation. Among radiologists surveyed, 69 percent felt DBNs increased patient anxiety about breast cancer, 74 percent said that DBNs increased awareness of the issue of breast density and mammographic sensitivity among patients and 66 percent said that they increased this awareness among radiologists.5 The results indicate that radiologists are still weighing the advantages and disadvantages of DBNs based on current standards. Many experts in the breast imaging community suggest that implementing new and more consistent national standards for DBNs could help women, and even some members of the medical community, better understand the impact of breast density.
Even with efforts to make the information in DBNs clearer and more consistent, it is important to remember that these communications are not meant to replace a conversation about breast density between a patient and doctor. Rather, DBNs should provide information that encourages a discussion about the risks of dense breast tissue and the optimal strategies to help women address these risks.
An Advanced, Appearance-based Solution
Coupled with efforts to improve communications with patients, advances in technology are improving our ability to assess breast density. The American College of Radiology (ACR) recommends the BI-RADS scale as a standardized system to categorize breast density when reading mammography, and instructs radiologists to include this information in the mammography report. But even with a standardized system, there can be significant reader variability because density categories are subjective and open to interpretation. A recent study published in the Annals of Internal Medicine confirmed that breast density assessments can vary significantly from one radiologist to another.6 Inaccurate results can lead to delays in getting patients the additional testing and appropriate treatment they need or can also result in patients getting tests that are not necessary.
Recent technological advancements could help overcome challenges associated with reader variability by providing a precise and consistent standardized density assessment. One new automated breast density solution uses an appearance-based approach in addition to assessing the volume of dense tissue (versus volume-based only) to deliver automated, rapid and reproducible assessments of breast structure, texture and fibroglandular dispersion. This technology automates the same analytical approach used by many radiologists. It analyzes digital mammograms, calculates the patient’s breast density and determines the appropriate density category corresponding to BI-RADS standards. Greater precision and consistency in measuring breast density can help identify more women at risk who can benefit from additional screening, while also helping many women at low risk to avoid unnecessary and costly medical procedures. For radiologists and medical practices, this technology can streamline workflow while providing higher levels of confidence in breast density reports.
The availability of cutting-edge technology that provides improved standardization in breast density assessments can lead to earlier and more accurate cancer detection in many women. Action to improve the quality of communications about breast density can encourage more women to discuss this important issue with their doctor and to make treatment decisions with improved comfort and confidence.
References
1 An Introduction to Dense Breast Tissue. DenseBreast-info.org. Accessed June 26, 2017. Retrieved from http://densebreast-info.org/
2 Sanders, Linda M. et al., Impact of the New Jersey Breast Density Law on Imaging and Intervention Volumes and Breast Cancer Diagnosis. Journal of the American College of Radiology, Volume 13, Issue 10, 1189 – 1194. http://dx.doi.org/10.1016/j.jacr.2016.05.005
3 Guterbock, Thomas M. et al. What Do Women Know About Breast Density? Results From a Population Survey of Virginia Women. JACR, 2016; 0(0). http://dx.doi.org/10.1016/j.jacr.2016.07.003
4 Kressin NR, Gunn CM, Battaglia TA. Content, Readability, and Understandability of Dense Breast Notifications by State. JAMA. 2016;315(16):1786-1788. doi:10.1001/jama.2016.1712.
5 Breast Density Legislation in New England: A Survey Study of Practicing Radiologists. Lourenco AP, DiFlorio-Alexander RM, Slanetz PJ. Acad Radiol. 2017 May 8. pii: S1076-6332(17)30174-5. doi: 10.1016/j.acra.2017.03.009.
6 Sprague BL, Conant EF, Onega T, Garcia MP, Beaber EF, Herschorn SD, et al. Variation in Mammographic Breast Density Assessments Among Radiologists in Clinical Practice: A Multicenter Observational Study. Ann Intern Med. [Epub ahead of print 19 July 2016] doi:10.7326/M15-2934
Roy Prager, M.D., is a radiologist practicing in New Jersey and Pennsylvania. He received his medical degree from State University of New York Downstate Medical Center College of Medicine and has been in practice for more than 20 years. He is certified by the American Board of Radiology.


 February 18, 2026
February 18, 2026 









