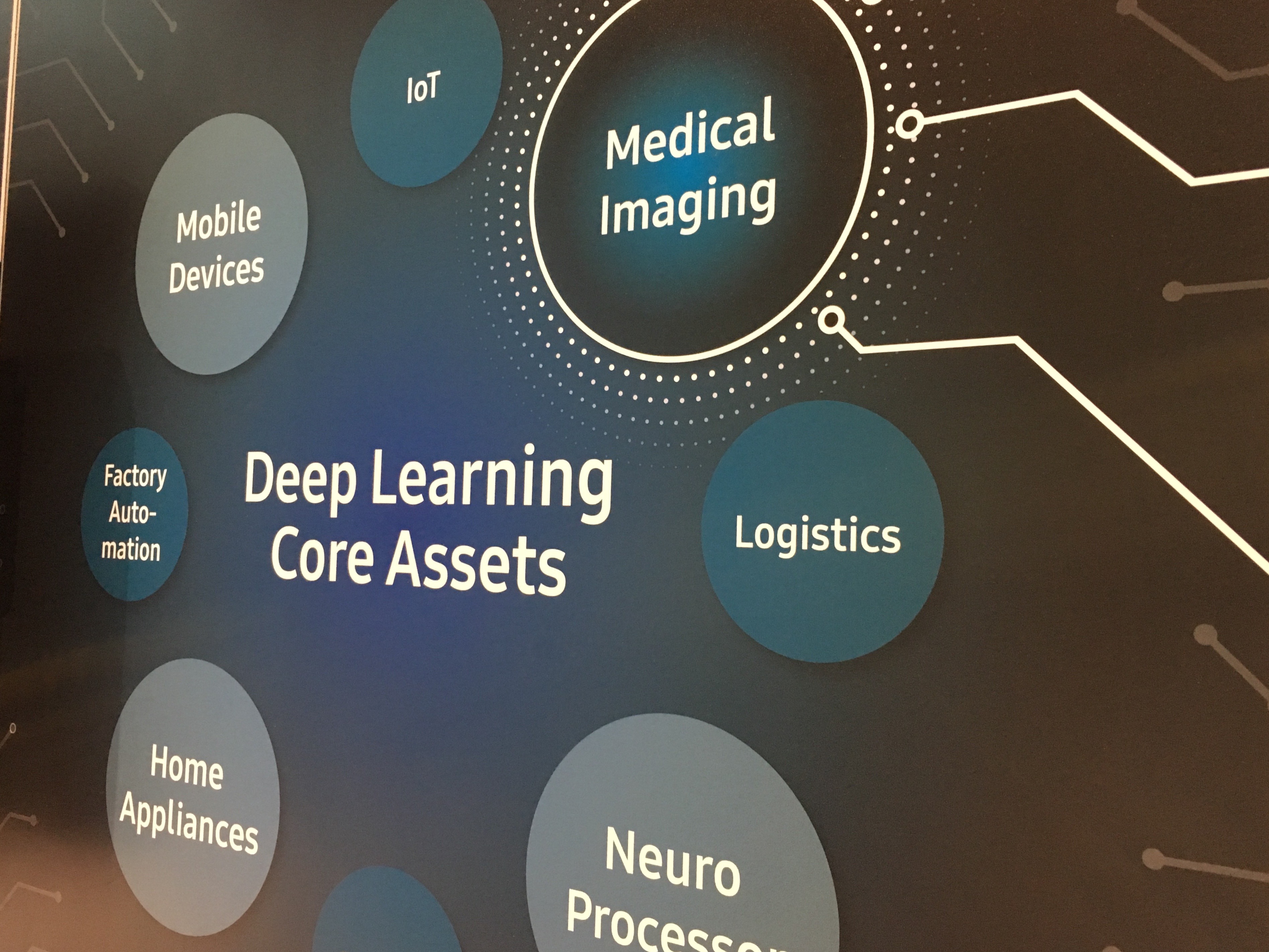
Deep learning, artificial intelligence in radiology was the prime topic of discussion at the RSNA/AAPM symposium at RSNA 2017.
When considering potential topics for the 2017 Radiological Society of North America (RSNA)/American Association of Physicists in Medicine (AAPM) Symposium, there was no question that it should address the growing excitement and concern surrounding artificial intelligence (AI).
One of the organizers, Paul E. Kinahan, Ph.D., vice chair of radiology research and head of the Imaging Research Laboratory at the University of Washington, Seattle, was interested in probing the convergence of radiology and AI and addressing some of the fears radiologists have voiced about the rapid growth of the technology. Many are wondering: will AI eventually render radiologists’ jobs superfluous and unnecessary?
“The answer to that question is clearly ‘no’,” said Kinahan. “On the other hand, aspects of artificial intelligence or deep learning or machine learning (ML) will certainly help elevate the productivity and accuracy of radiology.”
While there is often confusion over the terms, Kinahan said AI is essentially the simulation of intelligent behavior in computers, while ML refers to the algorithm or method used in AI. Deep learning is an area of ML research with the objective of moving ML closer to AI.
Kinahan moderated this year’s symposium, “Machine Learning in Radiology: Why and How?” was held Nov. 28 at RSNA 2017. Presenters are Keith Dreyer, DO, PhD, vice chair of radiology and director of the Center for Clinical Data Science at Massachusetts General Hospital in Boston, and associate professor of radiology at Harvard Medical School, and Antonio Criminisi, PhD, a principal researcher at Microsoft in the United Kingdom.
One issue Kinahan focused on during this year’s symposium was how AI fits into the whole big data question. “There’s lot of room for applying AI and machine learning methods to medical images themselves, but we would really like to see how we are able to integrate with the other data such as electronic medical records (EMRs) or pathology data for example,” he explained.
That type of integration is not without obstacles.
“We are deeply siloed into our own big data components, and radiology is one of the biggest,” Kinahan said. “How these big pockets of data get connected will almost certainly rely on assistance from artificial intelligence.”
While healthcare has been quick to adapt new technologies overall, that’s not the case with AI and ML, Dr. Dreyer said. “Healthcare has been late to the market in this area.”
Of course, incorporating AI or ML is easier said than done and presents a number of challenges — many of which Dr. Dreyer plans to discuss during his presentation, “Harnessing Artificial Intelligence.”
“It starts with raw data and constructing that information into data sets, applying the correct AI algorithms, creating models, testing inference engines that are created and validating them,” said Keith J. Dreyer, DO, Ph.D., FACR, chief data science officer, departments of radiology at Massachusetts General Hospital and Brigham and Women's Hospital. “Then we must translate them into clinical practice, go through regulatory approval followed by productization and commercialization.”
“Right now, we can count on one hand the number of AI medical imaging solutions that have made it through the FDA,” Dreyer explained. “And even fewer are in clinical practice, primarily because of the challenges involved.”
Antonio Criminisi, Ph.D., Microsoft’s principal researcher for AI, spoke about one of those solutions during his presentation, “Assistive AI for Cancer Treatment.” Quantifying the extent and size of a tumor such as a glioblastoma can be difficult, imprecise and time consuming, Criminisi said. But Microsoft’s InnerEye research project uses state of the art ML techniques to automatically detect, segment and measure both healthy tissue and anomalies, among other functions.
“AI-powered software tools like InnerEye will significantly reduce the time radiation oncologists need for radiotherapy planning,” Criminisi said.
The tool will also help radiologists track and measure the progression of cancer and other diseases and help surgeons plan complex surgeries, he added.
“This is the fruit of a decade-long research project that is now being translated into a practical and impactful software tool,” he said. “The aim is to increase the productivity of expert practitioners such as oncologists, radiologists and surgeons, while at the same time reducing costs for healthcare providers.”
Take an indepth view into AI products being shown on the show floor at RSNA 2017 in the VIDEO "Technology Report: Artificial Intelligence at RSNA 2017."
For more information from RSNA 2017 — Key RSNA 2017 Study Presentations, Trends and Video


 February 12, 2026
February 12, 2026 









