Breast cancer is the second leading cause of cancer deaths among women in the United States (2005-2009).
Breast cancer is the second leading cause of cancer deaths among women in the United States (2005-2009). Breast cancer deaths are going down the fastest among white women compared to women of other races and ethnicities. Black women have the highest death rates of all racial and ethnic groups and are 40% more likely to die of breast cancer than white women. The reasons for this difference result from many factors including having more aggressive cancers and fewer social and economic resources. To improve this disparity, black women need more timely follow-up and improved access to high-quality treatment.
Problem: Differences in screening, follow-up, and treatment.
Screening: Black women get mammograms as often as white women.
- Screening means looking for cancer before symptoms appear. Mammograms are the best way to screen for breast cancer. A mammogram is an X- ray picture of the breast.
- Black and white women reported equal breast cancer screening in 2010 (mammograms every 2 years for women 50 to 74: 74% versus 73%).(http://www.cdc.gov/cancer/breast/statistics/screening.htm).
- More black women are found to have breast cancer that has spread beyond the breast (45%) compared with white women (35%).
Follow-up: Black women get follow-up care later than white women.
- When a mammogram shows something is not normal, follow-up tests are needed to see if it is cancer.
- More black women experience follow-up times of over 60 days (20%) compared with white women (12%) after a mammogram that is not normal. Waiting longer for follow-up care may lead to cancers that spread beyond the breast and are harder to treat.
Treatment: Black women have different treatment experiences than white women.
- After cancer is found, treatment should start as soon as possible.
- Only 69% of black women start treatment within 30 days (compared with 83% of white women).
- Fewer black women receive the surgery, radiation, and hormone treatments they need compared to white women.
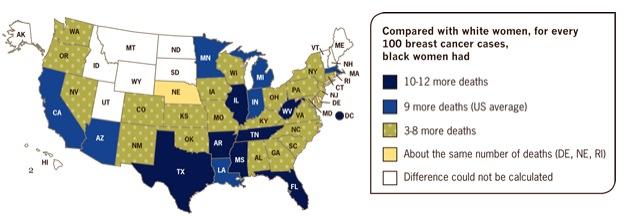
- Black women have 9 more deaths per 100 breast cancers diagnosed compared to white women.
What Can Be Done
Federal government is:
- Implementing the Affordable Care Act and educating women about the preventative benefits and coverage provided by the law, including coverage of mammograms without co-pays in many health plans and, beginning in 2014, the law will expand access to health insurance coverage for 30 million previously-uninsured Americans.
- Investing in the use of electronic health records and case management services in federally-funded health clinics so women get the timely followup care. For example, over $80 million were invested to help networks of health centers adopt electronic health records (EHR) and other health information technology (HIT) system.
- Supporting state efforts, through the National Breast and Cervical Cancer Early Detection Program, to help uninsured women get screening and access to treatment.
- Supporting research on health disparities in breast cancer.
State and local health agencies can:
- Use public-private partnerships to work with health care systems and health insurance companies to help educate women and their doctors about timely, high-quality breast cancer care.
- Use outreach strategies to help women understand why they need a mammogram.
- Educate women on what to expect when a mammogram finds something that is not normal.
Health care systems can:
- Engage well-trained case managers, health educators, community health workers and other patient navigators to help women understand and guide them through the health care system.
- Inform doctors about their screening and treatment rates to improve their timeliness of care.
- Explore strategies to enhance doctor-patient communications.
Doctors, nurses, and others who treat patients can:
- Make sure that women get recommended tests and treatments.
- Use tools like electronic systems or other reminders to notify patients when it’s time to get a mammogram.
- Continue to talk to women about their risk for breast cancer, explain test results and refer patients to specialists as needed.
Women can:
- Use these 10 questions to increase their communications with their doctor during appointments. (http://www.ahrq.gov/questions/tenquestions.htm).
- Get recommended mammograms.
- Contact their local health department or community health center for help if they cannot afford a mammogram. (http://www.cdc.gov/cancer/nbccedp/screenings.htm).
- Return for more tests if a mammogram finds something that needs follow-up.
- Ask about the kinds of treatment available.



 February 18, 2026
February 18, 2026 









