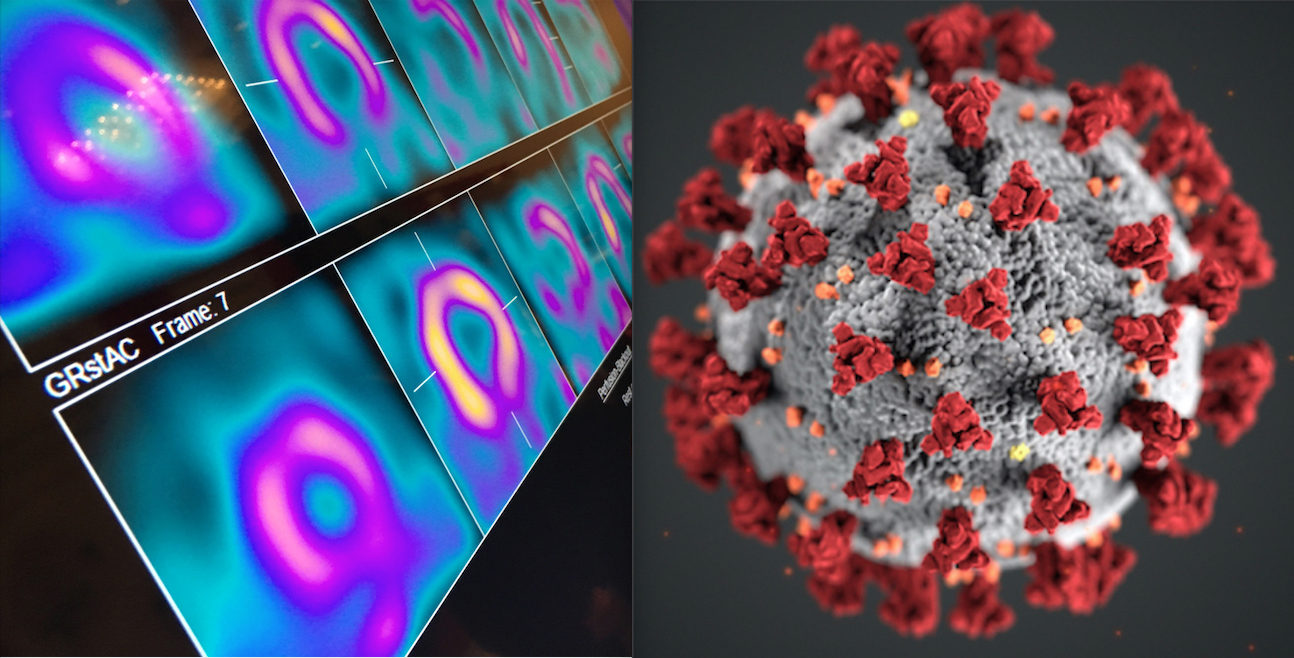
A year after COVID-19 turned the world upside down, the American Society of Nuclear Cardiology (ASNC) asked members how they are approaching the quest for nuclear cardiology lab improvement. The society wanted to know if the pandemic and its associated pressures led to changed priorities, or if some projects are taking a backseat to more pressing priorities.
The ASNC compiled the responses into the following list to share some of the strategies guiding nuclear radiology and cardiology teams at various healthcare systems in 2021:
1. Resolve to Muscle Through COVID-19
While COVID’s crisis point may have passed, in many parts of the world, the pandemic is going to be with us for a long time, members told the ASNC. And that, they say, means making peace with new processes and protocols, many of which were outlined by ASNC and Society of Nuclear Medicine and Molecular Imaging (SNMMI) in last year’s best practices information statements.
No matter what, the priority must be the safety of patients and staff. This was the prevailing theme in every conversation ASNC staff had while developing this story. So much so that they developed a related story “Coping with COVID-19 in 2021: Tips for Nuclear Cardiology Labs.”
Beyond the COVID-specific steps nuclear radiology teams will focus on for the next year or more is a mindset shift. This is what ASNC Past President Mylan Cohen, M.D., MASNC, calls “muscling” through.
“Continue to do the things that a nuclear cardiology lab needs to do to stay current, anticipate future demands, and continue to evolve,” Cohen explained. “We cannot abdicate our responsibility to pay attention to quality.”
The key to muscling through while continuing to improve your lab is picking one thing and going after it.
How to do that? By approaching the challenge like a coach would.
2. Think Like a Coach: Pick One Do-able Thing That Will Move You Forward
If you have ever been a coach, or been coached yourself, you have seen this tactic work. A good coach identifies a single thing that, if done even a little better, will move the team toward where they want to be, Cohen explained.
ASNC Board Member W. Lane Duvall, M.D., FASNC, echoes that idea while emphasizing that a team’s “one thing” need not be a formal study, complete with rounds of data collection and analysis. In the midst, or aftermath, of a crisis — when budgets might be tighter than usual — look for opportunities the crisis is presenting, he said. At Hartford HealthCare, his team’s focus on minimizing the time patients spend in the lab and optimizing social distancing evolved into “an opportunity to figure out a way to do more PET scans.”
“It wasn’t a formal QA project,” he noted, “but it was an opportunity to look at our processes and figure out how to improve them. If you don’t have a PET camera, your opportunity might be to maximize and make your SPECT protocols more efficient.”
No matter how small your one thing is, it must be selected thoughtfully. Assess your capabilities, the available resources, and account for financial and other limitations, Cohen said. Most healthcare systems took a financial hit last year, so an expensive undertaking might be off the table right now.
That does not mean you give up on your strategic priorities, Cohen added. His team had planned to join the ImageGuide Registry this year. They began the process, but then COVID-19 came along and it seemed the timeline might need to be changed. But that is not what happened.
“Enrolling in ImageGuide was something we recognize we must do at our center. It’s part of our quality effort, and it’s a high priority,” Cohen said. “So, despite the pandemic, we’re figuring out how to get it going. We may not have all of our readers enrolled initially, but we have to get started.”
Another selection strategy is to run with the opportunities the crisis brought to the fore.
3. COVID-19 Revealed Opportunities for Improvement. Seize Them Before You Forget Them
Hidden behind the many challenges brought by COVID-19 are opportunities, Duvall said. “Volumes might be down compared to what you’re used to, but this could provide an opportunity to look at how you could be doing things better or more efficiently.”
Asked for examples, Duvall brainstormed these suggestions:
• Stress-first/stress-only imaging: If keeping your waiting rooms clear means you’re seeing fewer patients and your staff are not as busy as usual, assign one staff member to screen patients who could be candidates for stress-first imaging.
• Review your protocols and processes: There may be untapped opportunities to reduce radiation exposure or adjust your weight-based dose protocols.
• Figure out what is behind your re-imaging rates: If there is downtime, work with your team to examine the times between injection and imaging as well as what is causing gut-uptake artifacts or patient motion.
Maria Costello, MBA, CNMT, NCT, director of nuclear/PET accreditation at the Intersocietal Accreditation Commission, said the IAC has been flooded with questions about what labs should be doing now. At its heart, her answer is the same as pre-pandemic: Concentrate on imaging each patient to the best of your ability within the limitations you have. She said a good tactic for right now is to focus on the technical quality of your images as well as the accuracy, completeness and timeliness of your reporting.
4. Consider Upgrading Your Nuclear Imaging Equipment
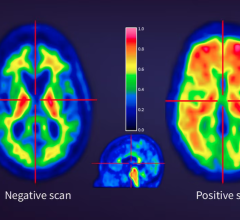
No doubt, the pandemic has forced varying degrees of recalibration all across healthcare. Perhaps now, when you are being asked to “pivot,” is the time to rethink the tools you are using. Samia Massalha, M.D., FASNC, of Rambam Healthcare, Technion Israel Institute of Technology in Haifa, said her team’s plan for 2021 is to implement viability testing using PET-FDG.
“So far, my center has been using thallium for viability testing,” she said. “We expect the switch will have a great impact on our workflow, the quality of our tests and on safety.” She is anticipating one-day testing that improves workflow; less ionizing radiation exposure to patients, staff and the community; and higher sensitivity and specificity of PET compared with SPECT.
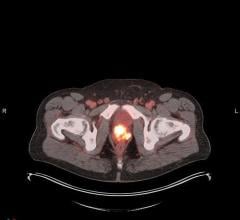
At the University of Pittsburgh Medical Center-Presbyterian, Lead Nuclear Cardiology Technologist Joseph Dietz, CNMT, expects similar shifts when his lab gets its first PET cameras installed this spring.
“It’s going to dramatically improve patient throughput,” he said. “We’re going to wait to see the impact on volume, but we may need to hire another nurse and possibly another technologist.”
His team is poised to undergo training on the new equipment and they are interfacing with UPMC-Presbyterian’s schedulers to make the most of PET’s time advantage. Compared to the 3- to 3.5-hour slots they reserve for patients undergoing imaging with their current CZT camera, they expect PET imaging appointments will take 90 minutes or less.
“It’s always a good thing when we can move faster for people,” Dietz explained.
When ASNC asked what advice he has for nuclear radiology and cardiology teams in 2021, Dietz pointed first to PPE and other COVID-19 safety precautions. He also urged labs to look at upgrading their A-SPECT cameras.
When UPMC-Presbyterian acquired its CZT camera in 2014, it was a game-changer. “With the older cameras, it could take as long as 5 hours to move a patient through,” Dietz recalled. “Most labs still have A-SPECT. Moving forward, they should get into the CZT cameras or cardiac PET just for the possibilities — plus it’ll make the cardiologists’, technologists’ and patients’ lives much easier.”
5. Take Advantage of ASNC Resources
Whether it is a single process change, a camera upgrade, or the shift from SPECT to PET, check out the resources ASNC already has. ASNC’s COVID-19 Resource Center includes pandemic-related resources including best practices information statements and archived webinars; tools for informing patients and referring colleagues about your lab’s safety measures; and links to COVID-19 advisor agencies, such as the CDC and FDA.


 February 03, 2026
February 03, 2026