May 29, 2019 — Out of more than 7 million current and former heavy smokers, only 1.9 percent were screened for lung cancer in 2016 despite screening recommendations, according to a new analysis. These numbers come despite U.S. Preventive Services Task Force (USPSTF) and American Society of Clinical Oncology (ASCO) screening recommendations.
This study, the first assessment of lung cancer screening rates since those recommendations were issued in 2013, will be presented at the upcoming 2018 ASCO Annual Meeting, May 31-June 4 in Chicago.
“Lung cancer screening rates are much lower than screening rates for breast and colorectal cancers, which is unfortunate,” said lead study author Danh Pham, M.D., a medical oncologist at the James Graham Brown Cancer Center, University of Louisville, Kentucky. “It is unclear if the screening deficit is due to low provider referral or perhaps patient psychological barriers from fear of diagnosis. Lung cancer is unique in that there may be stigma associated with screening, as some smokers think that if cancer is detected, it would confirm they’ve made a bad lifestyle choice.”
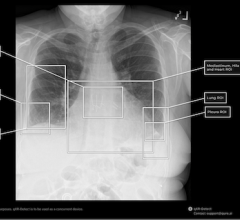
Lung cancer is the leading cause of death from cancer, with an estimated 154,040 deaths projected to occur in 2018 in the United States.1 The USPSTF recommends that people ages 55 to 80 years who are current or former heavy smokers (have smoked at least 30 cigarette pack-years) be screened for lung cancer using low-dose computed tomography (LDCT). Cigarette pack years are calculated by multiplying the number of packs of cigarettes smoked per day by the number of years the person smoked. In 2012, ASCO and the American College of Chest Physicians issued a joint guideline with these same recommendations.
The study’s researchers gathered data from the 2016 American College of Radiology’s Lung Cancer Screening Registry on people who received LDCT at nearly 1,800 accredited screening sites. They compared that data to 2015 National Health Interview Survey estimates of eligible smokers who could be screened based on the USPSTF recommendations. The analysis of the data was based on four U.S. census regions in the country: Northeast, South, Midwest and West. The screening rate was calculated by dividing the number of LDCT scans by the number of smokers eligible for screening per USPSTF recommendations.
The authors found that the South had the most accredited screening sites (663) and the highest numbers of smokers who were eligible for screening (3,072,095). Nonetheless, the screening rate in the South was only 1.6 percent, the second lowest in the country, whereas the West had the lowest rate at 1 percent and the lowest number of accredited screening sites (232). The highest screening rate was in the Northeast (3.5 percent), and the Midwest had the second-highest rate of 1.9 percent.
Nationwide, a total of 1,796 accredited screening centers could have screened 7,612,975 eligible current and former heavy smokers, but only 141,260 people received LDCT screenings (the nationwide screening rate was 1.9 percent). By comparison, about 65 percent of women age 40 or older had a mammogram in 2015.
Approximately 85 percent of the screened current smokers were offered smoking cessation resources, which was documented by providers prior to screening referral. The percentage of current and former heavy smokers offered cessation programs did not vary significantly by census region.
The authors have already started looking at 2017 lung cancer screening rates, and, preliminarily, there is a small overall uptick in screening rates in 2017 across all regions.
“This study makes a strong case that our country needs an effective public service campaign about encouraging lung cancer screening. Public service campaigns from the 1990s encouraged women to get mammograms, saving many lives in subsequent years. We need something similar to encourage current and former heavy smokers to get screened for lung cancer,” said ASCO President Bruce E. Johnson, M.D., FASCO.
For more information: www.asco.org
Related Lung Cancer Content
Physicians, Patients Talking Less About Lung Cancer Screening
VIDEO: Radiation Versus Surgery for Non-Small Cell Lung Cancer


 March 05, 2026
March 05, 2026